the maskers comic presents
Writings and Resources
on covid-19 prevention
Join us as we look into all the latest information with links to sources to help you decide how to protect yourself and your community.
Infection Control Policies (Healthcare/ HICPAC/CDC) October 2024
Is COVID-19 Still Considered Dangerous? July 2024
CDC Isolation Guidance Not Supported. Minimum 14-day Isolation Period Needed April 2024
Email Campaign Against Anti-Mask Bills June 2024
Infection Control Policies (Schools) March 2024
Why We Mask January 2024
Clear Public Health Messaging on Multiple Layers: Beyond the Swiss Cheese October 2023
The Maskers Blog
IS COVID-19 STILL CONSIDERED DANGEROUS?
By Shea O’Neil 7-5-2024
Yes! It is dangerous in both its initial infection phase as well as its long-term phase.
"COVID-19 is a serious threat to the long-term health and well-being of people and it should not be trivialized." -- Ziyad, Al-Aly, MD, a Washington University clinical epidemiologist and a global leader in long COVID research.

WHAT IF I'M VACCINATED!?
Vaccines have many benefits but fall short as a solution to COVID-19 risks. Vaccinated people can still get infected with COVID-19, spread it to others, and get long-COVID.
A landmark 2022 study shows vaccines give only a modest risk-reduction (15%) for long COVID when comparing vaccinated to unvaccinated individuals. A 2023 study shows 10-12% of cases amongst vaccinated people result in long COVID.
Many have no or limited vaccination protection, such as persons who are not vaccinated due to allergic reactions or other medical contraindications, medical mistrust, avoidance due to risks of developing conditions or other adverse reactions to the vaccines, those with immunosuppression from other conditions or medications, and those who are not up to date with vaccinations. The percent of the US population reporting receipt of the updated 2023-24 COVID-19 vaccine is only 13.7%.
Besides not giving adequate protection from long COVID, vaccines alone cannot slow down the evolution of the SARS-CoV-2 virus and need to be supplemented with preventative measures such as masks and air filtration that significantly reduce transmission in the population. Vaccines cannot keep up with newer variants that evade prior immunity from either infection or vaccination or both. Vaccine’s effectiveness in preventing infection has shown to wane significantly over time.
A recent study shows progressive loss of neutralization (that is loss in the ability to block the entry of the SARS-CoV-2 virus into a cell in order to prevent infection and replication) observed across newer variants, irrespective of vaccine doses. It particularly notes that although the updated XBB.1.5 booster significantly increased titers against newer variants it did NOT show to be effective against JN.1 variants. JN.1 variants and their offshoots are the most prevalent variants in the US currently as of July 2024. Without mitigations, variants will continue to evolve faster than vaccines can keep up with. The result will be more COVID-19 infections and more long COVID cases, and the associated physical, economic, and social costs, as we will see below.
LONG COVID IS not rare, cases are rising, and science is showing chronic, serious, and debilitating outcomes
Long COVID IS NOT RARE-- More than 17.6 million people in the US alone have been diagnosed with long COVID, and more than 65 million globally. Both of those numbers are considered likely underestimates. To put that into perspective, when looking at new cases in the US over the past 4 years, long COVID cases are more than double the amount of new cases of ALL TYPES of cancer combined, with new cancer diagnoses being approximately 8 million over the past 4 years compared to 17.6 million new long COVID cases over the past 4 years.
Long COVID continues to be serious and prevalent amongst all populations. According to a 2023 Nature article, “long Covid incidence is estimated at 10–30% of non-hospitalized cases, 50–70% of hospitalized cases and 10–12% of vaccinated cases …Symptoms can last for years, and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong. With significant proportions of individuals with long COVID unable to return to work, the scale of newly disabled individuals is contributing to labour shortages. There are currently no validated effective treatments.”
A 2021 systematic review found more than half of COVID-19 infections resulted in long COVID six months after recovery. A 2024 Review of organ damage from COVID and Long COVID: a disease with a spectrum of pathology states that “organ damage might affect over 50 % of post-COVID-19 individuals, and perhaps more in adolescents and children “. A 2023 Nature immunological review concluded “The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it. If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID.”
Long COVID can be serious and debilitating, often reported to impact life worse than cancer and other diseases. Intense fatigue and "brain fog" (a term some say is too mild and should be referred to as brain damage) from long-COVID was rated worse than those recovering from stroke, and similar to that of Parkinson's disease. Recovery remains rare. It affects all ages and demographics.
Kids have been shown to be much more susceptible to Omicron infections than prior variants, with resulting damage to their lungs, immune systems, increased risk for diabetes, and systematic review showing a 1 in 5 chance of children getting long COVID. A Lancet study found the long COVID risks to be between 20-30% in children.
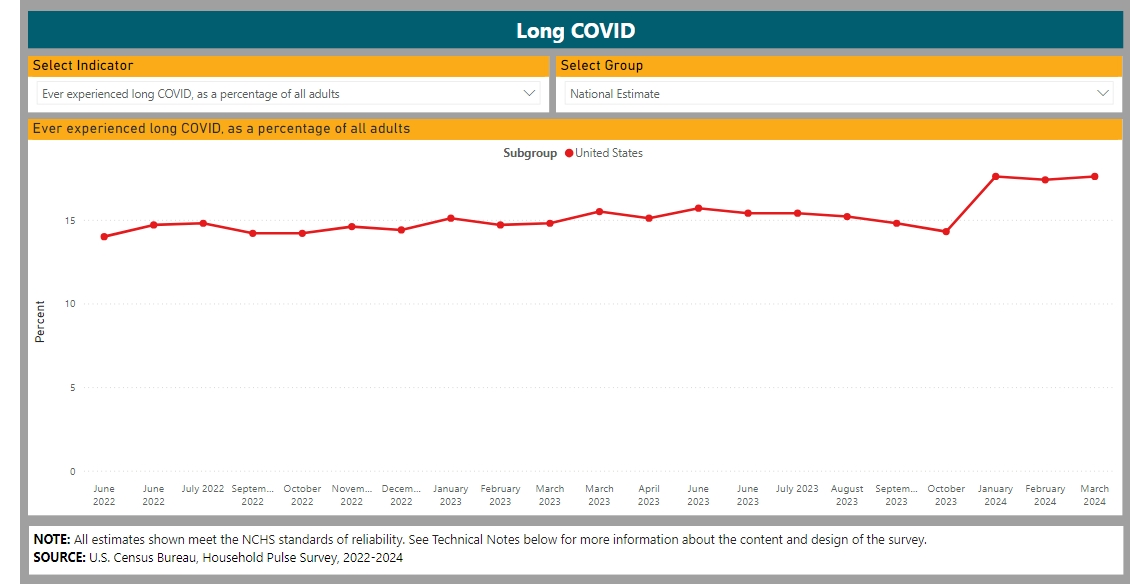
Furthermore, research and data from the CDC's Long COVID - Household Pulse Survey - COVID-19 (cdc.gov) (see chart below) shows that Long COVID is not slowing down, it is rising. Data shows that long COVID is surging in the US, and across the globe.
COVID REINFECTIONs are common, and each reinfection makes LONG COVID MORE LIKELY
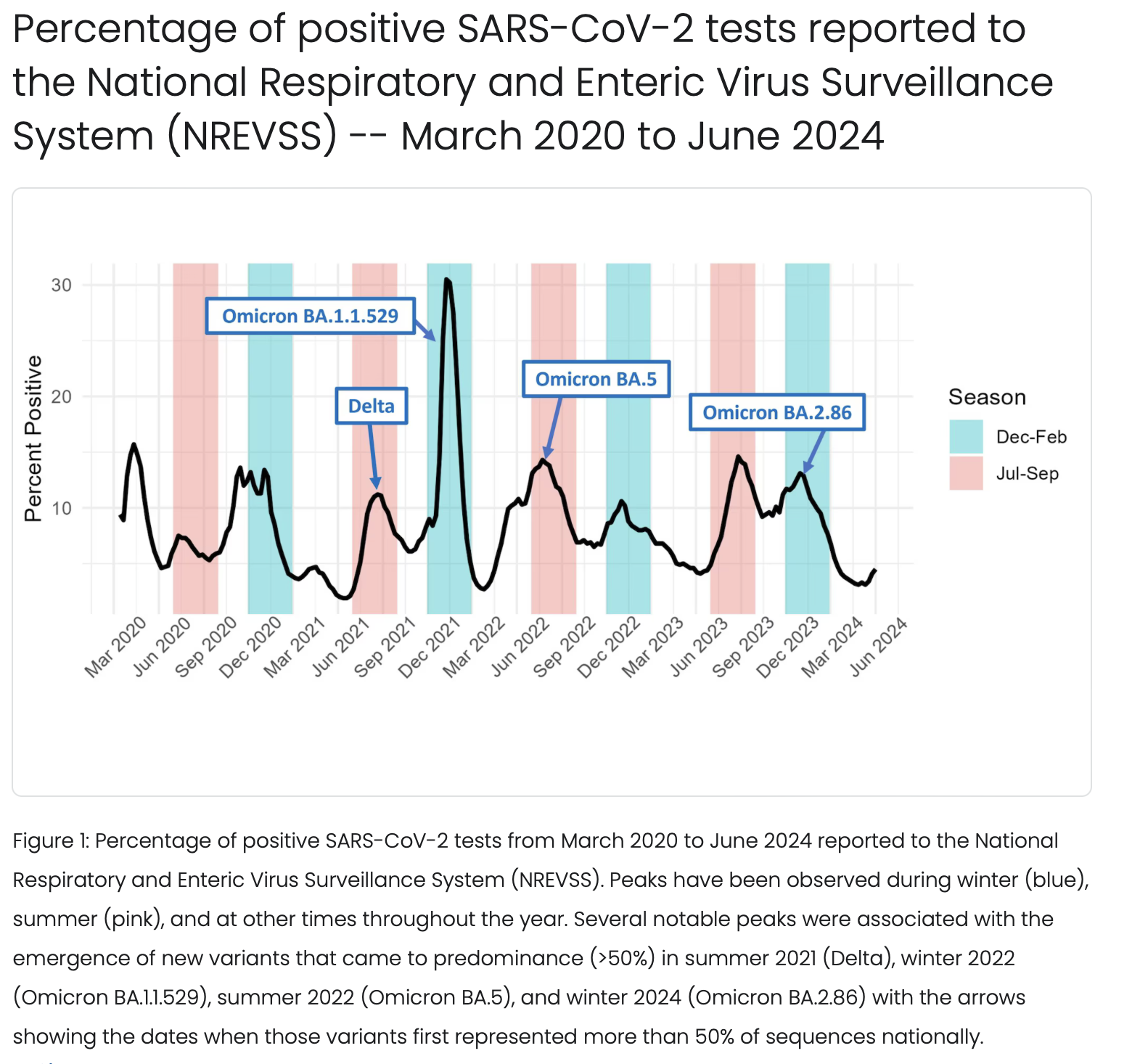
COVID-19 is a year-round threat, with exceptionally high surges during times of high travel and indoor gathering without precautions like masking and air filtration to mitigate effects. The spread of newer immune-evasive variants, with nothing to stop them, has made to reinfections common.
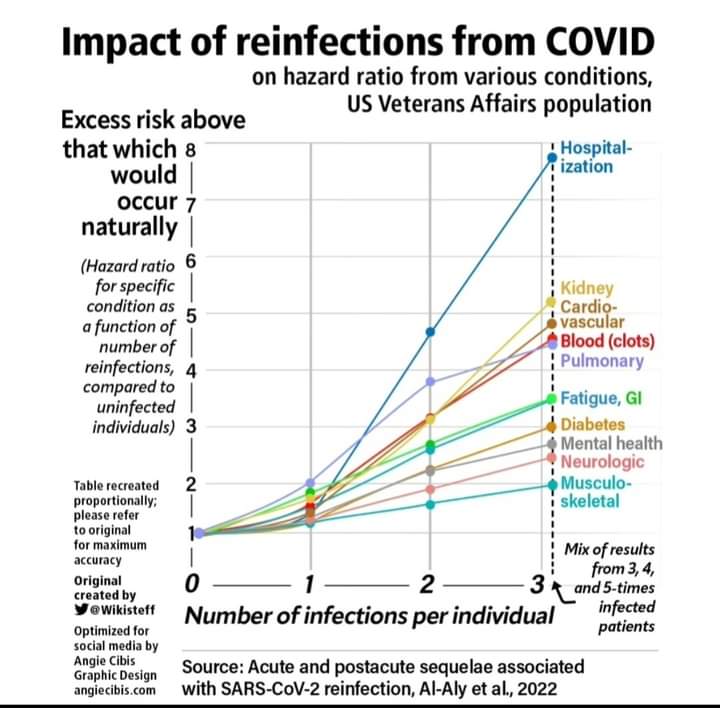
Furthermore, studies show risks for serious short- and long-term health problems increase with each reinfection. A 2022 Nature study shows the excess health risks above what might naturally occur increases significantly with every reinfection:
A 2023 study on long COVID among Canadians showed that: "on those who reported ever experiencing long-term symptoms, those who continue to experience these symptoms (58.2%) outnumber those who have reported them resolved (41.8%).
Long COVID causes serious complications, often chronic, with negative health impacts including disability and death. A 2023 Scientific American article stated “the most common, persistent, and disabling symptoms of long COVID are neurological”, later quoting a physician saying, “I now think of COVID as a neurological disease as much as I think of it as a pulmonary disease, and that's definitely true in long COVID.” Although formal guidance on how to record long COVID on death certificates was not released until 2023, CDC data from early 2024 has shown thousands of deaths of US citizens from long COVID.
The effects of long COVID have and are continuing to show up showing up in steep increases in disability rates in the workforce since 2020, as can be seen in the image below:
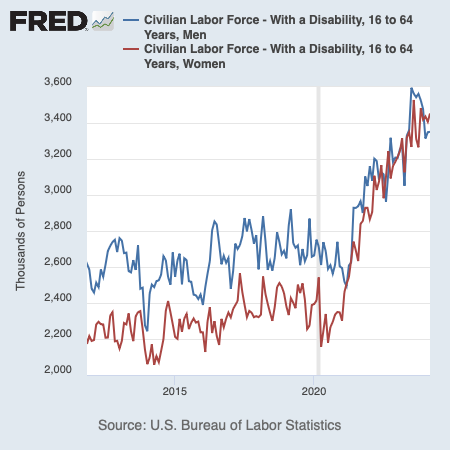
A 2022 Brookings Report shows that long COVID is keeping over 4 million people out of work so far. This impact is not set up to lessen any time soon, due to the continued spread of COVID-19 and the worsening effect of infections and reinfections on the body.
LONG COVID IS NOT MYSTERIOUS– WE KNOW THE LIKELY CAUSES AND CAN SEE THE EFFECTS CLEARLY
A 2023 study indicates likely causes of long COVID include:
persistent SARS-CoV-2 virus lingers in the body that remain long after the initial acute infection causing cascading effects on multiple organs systems.
reactivation of latent viruses: (viruses that are common but dormant in our bodies) will become activated and cause problems and chronic diseases
chronic inflammation in the organs, blood vessels, and immune system
Inflammatory enzymes that cause inflammation and can manifest into a wide variety of long-term health conditions.
Researchers in a 2024 study found major differences in different long COVID groups, including:
GI (gastro-intestinal) and cognitive long COVID groups with more associations between Epstein–Barr virus reactivation and neurological symptoms, autoantibodies and GI symptoms, as well as finding brain–gut axis disturbances more common in the GI group.
The Cognitive group had more signatures suggestive of neuroinflammation (C1QA), consistent with findings of brain abnormalities on magnetic resonance imaging.
The cardiorespiratory group showed domination of proinflammatory signatures. Lung-specific inflammation was suggested by the association between PCDH1 (an airway epithelial adhesion molecule and cardiorespiratory symptoms.
Fatigue and anxiety/depression groups had signatures that were consistent with those seen in non-COVID depression, suggesting shared mechanisms including associations between markers of myeloid inflammation enhancing immunopathology and fatigue.
In February 2024, researchers in Dublin, Ireland published a study in Nature Neuroscience that found that:
"sustained systemic inflammation and persistent localized blood–brain barrier (BBB) dysfunction is a key feature of long COVID-associated brain fog."
blood vessel inflammation and blood clotting issues resulting in microbleeds in the brain.
inflammatory biomarkers suggesting immunological dysfunction.
structural brain damages in regions involved in "brain fog"--an umbrella term for the fatigue, memory, and cognitive problems described by many with long COVID.
brain abnormalities to be similar to patients suffering from neurological diseases including epilepsy, traumatic brain injury, and schizophrenia, and
other biomarkers similar to those implicated in the pathogenesis of chronic fatigue syndrome, a condition with clinical similarities to long COVID. The researchers found no difference in age in this study, again affirming that long COVID is happening to people of all different ages.
A 2024 Lancet study showed that cognitive symptoms and brain abnormalities were still present 2 years after infection. Another 2024 study found that a year after COVID infection, 7% of children still experienced cognitive problems.
One thing is certain, we know enough already about COVID-19 to know it is causing serious, significant, wide-ranging effects on health, and no subgroup has been found to be immune from those risks: every age, class, race, religion, and health status are at risk, and the only way to prevent long COVID currently is to not get infected to begin with.
THE 2024 us department of defense report
The US Department of Homeland Security released a COVID-19 Report to the public in January 2024. Some key admittance included in the report:
INFECTIVITY : Decreased threshold for infectivity has been modeled in newer variants, suggesting SARS-CoV-2 infection can occur from 100 virus copies of Omicron variant.
TRANSMISSIBILITY: As of 1/22/2024, COVID-19 has caused at least 774,075,242 infections and 7,012,986 deaths globally. In the United States 1,169,666 deaths have been confirmed. Cases and fatalities are likely underestimated.
SEVERITY: COVID-19 is more severe than seasonal influenza, evidenced by higher intensive care unit (ICU) admission and mortality rates. In the U.S., 29-34% of hospitalized patients required ICU admission, and 12.6-13.6% died from COVID-19. COVID-19 also causes pneumonia, cardiac injury, kidney damage, pancreatitis, arrhythmia, sepsis, stroke, respiratory complications, and shock. SARS-CoV-2 weakens blood vessels in the lungs and is associated with hyperactive platelets, leading to ARDS. Clotting affects multiple organs and is present in 15-27% of cases.
LONG-TERM EFFECTS: Long COVID is a multisystemic illness, where symptoms linger for weeks, months, or years after initial diagnosis of COVID-19. The incidence is estimated at 10-30% for non-hospitalized cases, 50-70% for hospitalized cases, and 10-12% for vaccinated cases. The incidence rate of pediatric long COVID is still uncertain. Due to small study sizes and inconsistent collection and analysis methods, the reported incidence rate can vary from approximately 25% to <5%. A study determined that age, sex, and vaccination status could not be used to predict the development of long COVID.
DISEASE CONTROL: NPIs (Non-pharmaceutical Interventions) should be implemented in conjunction with vaccination. NPIs and vaccines work synergistically to reduce disease burden, and both are needed when vaccine coverage rates are low. Early in the pandemic, NPIs were responsible for a 35% reduction in transmission, while vaccinations were responsible for a 38% reduction in transmission; however, when NPIs were combined with vaccination it resulted in a 53% reduction in transmission. Modeling shows that NPIs can reduce the likelihood of vaccine-resistant variant emergence, as the simulated emergence of vaccine-resistant strains was highest when vaccination levels were high (60%), but transmission was uncontrolled. Researchers have proposed an Omicron variant model to provide insights to coordinate NPIs and vaccination, where NPIs become more important to control transmission as the vaccine efficacy is reduced due to the emergence of new variants.
PREVENTATIVE MEASURES: Face masks inhibit transmission by both reducing the number of exhaled particles from infectious individuals, as well as reducing the number of inhaled particles when worn by uninfected individuals. A large analysis across 56 countries found that mask wearing reduced the mean transmission rate by 19%. In a study of K-12 school districts across nine states, those with universal masking policies reported 3.6 times fewer secondary infections than those with optional masking policies. Reducing capacity at crowded indoor locations, increasing indoor air flow rates, adding portable air cleaners, and wearing masks may reduce indoor transmission. Aerosol infection risk is not uniform in indoor environments, and can be greatly impacted by patterns of ventilation.
THE 2024 senate hearing on long covid
On January 18th, the Senate Health, Education, Labor, and Pensions (HELP) Committee held a hearing titled "Addressing Long COVID: Advancing Research and Improving Patient Care." Here are the highlights:
Senator Sanders began the hearing stating long COVID affects all age groups and backgrounds. The strange and debilitating symptoms include serious neurological and cardiovascular effects, and that these can last weeks, months, and years, often becoming chronic. With no FDA approved treatments for long COVID, Sanders contends, there is an urgent need for action. Sanders goes on to state that long COVID is not a minor inconvenience but can affect people's ability to work, care for families, and live full lives. Currently more than 16 million in the US have long COVID, more than 4 million are out of work because of it, and it costs us more than $170 billion dollars a year.
Senator Markey called the numbers "staggering", stating according to NIH, “out of the people who have had COVID, 22-38% of them are experiencing long COVID, and that may be an underestimation”. He went on to say people “should be masking, they should be getting vaccinated, because there is a high probability they will have long COVID”, and that “it is imperative that we provide funding for research”.
The witnesses at the hearing– patients and caretakers of those with long COVID– spoke of the difficulties accessing care and treatments due to professional ignorance on long COVID, even after tests showing real physical damage were often brushed aside or dismissed as just being anxious. They spoke of the need to include patient voices, lived experiences, and continuing education in the process of expanding education to medical professionals.
Senator Romney, who has a family member with long COVID, acknowledged the severity and long-term nature of symptoms including micro blood clots and the associated aches, pains, and fatigue. He asked with frustration, "What are we doing to prevent it?"
Senator Murray acknowledged the need to improve public health infrastructure as well as increase public awareness to help with prevention. Murray also inquired on the challenges navigating our healthcare system and the need at the federal level to expand access to quality care for long COVID patients. Senator Hassan said long COVID patients are often spending $9,000 annually for out of pocket costs, and that medical providers who treat long COVID have huge waits already. Senator Braun said, “No one should go broke in this country because they get sick or have an accident”, with a reception of applause from the audience (many of whom were wearing high quality masks).
There was also an expert testimony, in which lead doctors, scientists, and researchers gave input– including Dr. Hawkins, an ICU doctor turned long COVID clinical trial runner, and Dr. Al-Aly, a well-renowned physician-scientist whose works have led the research on long COVID.
We have “zero treatments” approved for long COVID Al-Aly said, as he wore a well-fitted respirator mask, “Now you should be asking me how we prevent long COVID, and the only way to prevent long COVID is to prevent COVID infection in the first place”.
He goes on to stress how we do not have vaccines that block infections right now, and we need them to be developed and to last. But we do have ventilation and filtration technologies we can put into place to reduce risks.
He continues by saying, “Acute infection can cause long-term disease, it can end up disabling people,” warning, “Even if people managed to emerge unscathed after the first infection, they may get long COVID after reinfection.” Al-Aly testified to the senators: “The risks of getting long COVID after reinfection are not known to the general public”, which hinders their ability to give a response that matches the severity of the problem.
IF IT HASN'T GOTTEN ME BY NOW, DOESN'T THAT MEAN I'M IN THE CLEAR?
If you haven't had any long-term effects after your first infection, and/or if your first infection was not severe, it does not mean you will not in your second, third, or fourth. Most people suffering from long COVID had mild initial infections. As we have seen above, initial (aka acute) infection risks are only a small part of COVID-19 infections, and health risks continue long after this time period. Because long COVID symptoms often do not appear until months after infection, many fail to connect their long COVID symptoms to their initial COVID infection-- which may have even been asymptomatic. Research shows that asymptomatic infections are not only transmissible to other, but they can also result in long COVID. A 2021 study showed one-fifth of people with asymptomatic COVID-19 infections end up developing long-lasting symptoms.
There is no long-term immunity to COVID-19, and reinfections with new variants are common whether you are vaccinated or not. Infection-gained immunity has proven to be short-lived. A recent Lancet study shows that reinfections are actually more likely AFTER prior Omicron infection (not less). There is also a growing body of research on long-term COVID-caused immune damage.
KNOW YOUR RISKS: SHORT-, MEDIUM-, AND LONG-TERM
One cannot truly make a decision about what to do in regard to COVID-19 without being informed of the risks involved, from immediate to long-term.
We know COVID-19 risks move well past the acute infection-- the term for the initial "sick" phase that now is resulting in less deaths and hospitalizations than earlier in the pandemic, but still is killing over 1,000 Americans each week, even in Spring 2024. The COVID-19 death rate is at least 4 times higher than influenza. It has killed more than 1.2 million people in the United States and more than 7 million world-wide. To put it in context, 1.2 million is the same amount of military fatalities in all major wars from 1775 to 2024. At this rate, we will run out of space on the COVID memorial wall soon just considering deaths during the acute phase of infection alone!
However, it isn't even the hospitalization and death rate in the acute infection that is our most likely risk (even though it IS a concern, as more than half of the US population is considered higher risk for severe outcome from COVID-19).
Yet, there is an even greater chance that this will affect our long-term health in serious, often chronic and disabling ways, and those risks pertain to ALL people, whether one is considered higher risk in the acute infection phase of the disease or not. A recent study shows that a quarter of infections result in SARS-CoV-2 virus persisting in people's blood, and many studies show the virus can wreak havoc on the body and its systems, with serious and even deadly health effects.
Heart Attack and Stroke Risks In the Short and Long-Term
Some of the most serious and deadly risks are related to heart attack and stroke risks in all ages. A 2023 study in Nature Cardiovascular Research shows the virus infects coronary arteries, causing plaque buildup to become inflamed and break off, which can then lead to a heart attack. A 2022 study confirmed stroke risks were heightened in younger and healthier people, including those with seemingly mild acute infections. COVID-19 infection more than doubles heart attack and stroke risks for up to a year after infection. They are exceptionally high in the weeks after infection. A 2021 Lancet study shows heart attack risks are 3-8 times higher, and strokes caused by blood clots 3-6 times higher, the weeks after COVID infection. Vaccination helps reduce some of these effects, while showing no effect on others.
A study on the cardiac effects of COVID-19 shows heart effects at four different time windows after infection: 0–30 days (namely the acute phase), AND 31–90 days, 91–180 days and 181–365+ days (these last three comprise the post-acute phase). The researchers found that although some of the heart risks during the acute phase were lessened by vaccination, most of the long-term risks were heightened after COVID infection whether you were vaccinated or not. They found:
a substantial reduction of risk (45–81%) for thromboembolic and cardiac events in the acute phase of COVID-19 associated with vaccination.
A lesser reduction (24-58%) for the risks for post-acute COVID-19 VTE (venous thromboembolism), ATE (arterial thrombosis/ thromboembolism), and HF (heart failure).
No reduced risk for post-COVID-19 MP (myocarditis/pericarditis) and VACA (ventricular arrhythmia/cardiac arrest) in vaccinated people was seen after the acute phase.
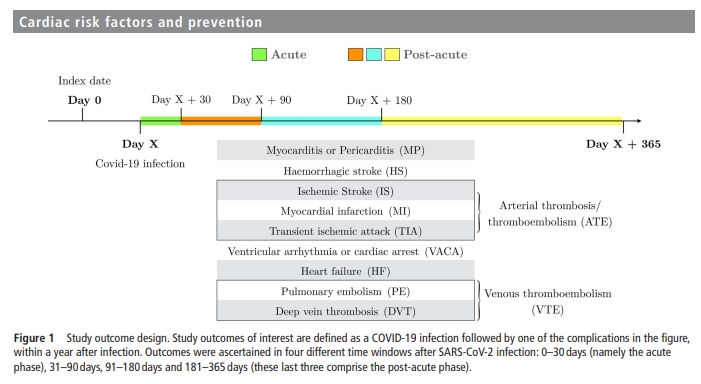
Figure Above shows how researchers often look at different risks of COVID during different time periods of the acute and post-acute phase.
Long COVID heart attack and stroke risks are thus a problem whether you are vaccinated or not, and are far worse than long-term risks after other viral infections, such as the flu. Even though scientists are learning more that flu can also cause inflammation that increases heart and stroke risks, research shows that SARS-CoV-2 virus does so at rates more than 7 times higher than after the flu.
And, the long-term effects of COVID-19 infection can move well beyond heart attack and stroke risks.
Other Long-Term Risks and How COVID Causes Them
COVID-19 infection can cause long-term gastrointestinal problems, multi-organ impairment, abnormalities of blood vessels and coagulation, mitochondrial cell dysfunction, functional impairment and fatigue, muscle abnormalities, development of allergic diseases and asthma, immune dysregulation, detrimental neurological impacts (including brain cell fusion, depression, and cognitive impacts), as well as many other post-acute infection health effects (all under the umbrella terms "long COVID" or "PASC" (Post-Acute Sequelae of COVID-19).
Because long COVID is so diverse depending on which part(s) of the body are affected, it is now being divided into (sometimes overlapping) subtypes, based on its cause and/or the parts of the body it affects. By defining subtypes, healthcare professionals and researchers may be better able to identify long COVID, and/or develop treatments. But right now, there are no approved treatments or cures for long COVID.
protecting oneself is not a solo act
Respirators, like N95, KF94, KN95, or better, along with cleaning the air, are non-invasive ways to filter out the SARS-CoV-2 virus from the air, making it much more difficult for it to infect you. And yes, we can filter out the virus. We have plenty of studies and real-life examples on the efficacy of N95 masks in filtering out aerosols like those the SARS-CoV-2 virus travels on when it enters your nose and mouth, and many industries use respirator masks, from firefighters fighting wildfire smoke, to people spraying pesticides, to carpenters using power saws to cut wood. They can capture tiny particles INCLUDING those that the virus travels on.
Wearing a respirator mask (N95, KN95, KF94, or better) as opposed to a surgical mask makes a huge difference. In a real world study on the efficacy of respirator masks in a COVID ward, when surgical masks were replaced with FFP3 (N95) respirators for nurses on a COVID-19 ward, infection risk declined by 52%-100%. It has been stated for decades that surgical masks are not good for things like wildfire smoke (aerosols), and to wear respirator masks. And, unlike early on in the pandemic, respirator masks are widely available now in most countries, although more efforts should be made to make them accessible world-wide to all people.
A pre-COVID study showed respirator masks significantly reduced infections with airborne pathogens, also showing continuous use of respirators to be more effective than intermittent use.
A 2021 report published in Science concludes face masks effectively limit the probability of SARS CoV-2 transmission, while also acknowledging that mask efficacy depends on airborne viral load, adequate fit and filtration, and other protections used.
Masks work better at lower viral densities. Respirator masks sometimes may have gaps, leaks, or times where we take the mask off for various reasons. Fit test kits can be expensive, and most people are wearing non-fit tested masks. Even just one infected individual can expel a high amount of virus into the air. Having more people masking, reducing the number of infectious people in a space, adding enhanced filtration of the air, reducing the density of people in a space, and decreasing time in higher risk situations that are lacking in any one of these areas, are all important.
In the image below from Sanford Health, you can visualize how the risks of COVID-19 infection and transmission decrease with more people masking. When the non-infected person is the only one wearing a mask, the chance for infection is still high:
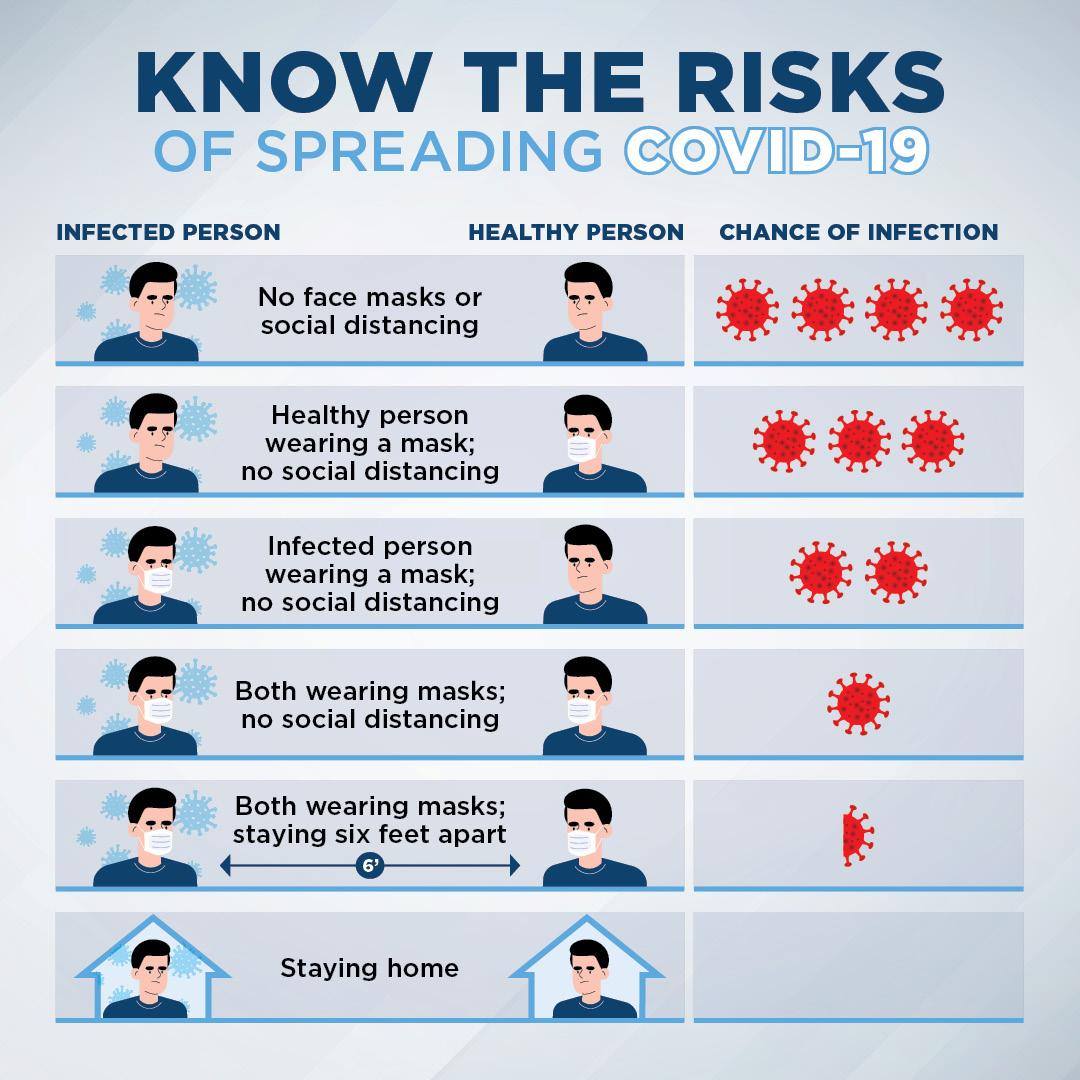
A 2021 PNAS study found that when:
only the non-infected person wears a surgical face mask, with an infectious person speaking at a distance of six feet, the risk for infection reaches 90% after 30 minutes.
With only the non-infected person wearing an N95 respirator mask in the same situation, infection risk remains at approximately 20% after one hour.
When neither wears a mask the risk of the infectious person transmitting to the non-infected is 90% after only a few minutes.
However, when both wear a well-fitting N95 mask, infection risk is only 0.4% after an hour. (Note: newer variants are even more infectious than the variants that were around when this study was done, meaning time to infectious dose may be less than these estimates).
It is really important for us to advocate for others to mask along with you when sharing air-- ESPECIALLY in spaces we have to spend more than an hour of time in. Even 20% risk of getting COVID-19 is too high, and that is just for 1 hour of me one-way masking, using the estimate from the study above (that was made with LESS contagious variants than what is circulating now-- meaning the risk is likely higher than 20% after 1 hour of one-way N95 masked at 6 feet distance exposure).
It is also important to keep the mask on. According to a 2023 study, transmission can happen in as little time as 20 seconds to 4 minutes. A Nature study from December 2023 also showed transmission can happen in as little as a few minutes in normal conditions. If one person has to unmask for a quick drink of water, it is really helpful when others are wearing a mask and not in close proximity to the unmasked person. Spreading out outside to eat, or making arrangements to eat at home instead of in indoor or crowded outdoor settings can be helpful.
Adding infection prevention strategies to incorporate universal masking and enhanced air filtration makes huge a difference. A 2021 study showed universal masking is significantly better than one-way masking. And research shows adding mask requirements reduces the spread of COVID-19.
Wearing masks will advance our fight against COVID-19 by reducing infections and slowing down its evolution, making the vaccines and treatments we do have more effective for longer periods of time.
A 2022 research article found that the mean observed level of mask wearing corresponded to a 19% decrease in the reproduction number (a measurement of how many people each infected person spreads COVID-19 to) , and stated that “the evidence that mass mask wearing reduces transmission implies that mandates (and other mask-promotion policies) may be effective against COVID-19 if and when they improve or increase the use of masks.” Adding increased air filtration also makes a difference. A 2022 study published in the Journal of Infectious Diseases found that fit-tested N95 mask combined with a portable HEPA filtration system offers the best protection against viral particles in the air.
Multiple Layers and Clear Public Health Messaging
We give more information on these all of these topics in our Multiple Layers: A Step Beyond the Swiss Cheese Model, where we also discuss the importance of clear public health messaging, such as the importance of openly acknowledging and expressing the risks of COVID-19 and long COVID, the need to push for political action, and the need for policies that prioritize public health over short-term economic interests. We also talk about the important responsibility of each individual and organization to develop effective strategies on how to prevent COVID-19 in our homes, schools, workspaces, and communities, and take a look at how to properly use the tools we have to prevent infection.
We all deserve to be given the information and tools we need to keep ourselves and others safe, while also being social. Creating that opportunity is what this website is all about.
So, in short, is COVID still dangerous? Yes! Yes, it is.
Can we do something about it? Yes, we can.
The Maskers Comic Presents
CDC's Isolation Policy strays further from the science
CDC's 2024 Updated Isolation Guidance Not Supported. Minimum 14-day Isolation Period Needed.
By Shea O’Neil, last edited 4-23-24
The CDC updated their Isolation Guidance this March 2024, straying from the current research on COVID-19, and making recommendations that endanger the public by encouraging contagious people to return to normal activities–such as work and school– while proposing inadequate compensations for the increases in infectious people in buildings.
In their updated guidance the CDC recommends that people stay home and away from others until at least 24 hours after both their symptoms are getting better overall, and they have not had a fever (and are not using fever-reducing medication). The guidance admits that people may still be contagious, saying: "Since some people remain contagious beyond the “stay-at-home” period” they encourage “added precaution over the next five days.” For higher risk people, they state: “Since it may take people with weakened immune systems longer to recover from respiratory viruses, this may influence choices on precautions after returning to normal activities following time at home sick” but fails to give guidance beyond that on how to protect themselves and others.
The “added precautions” they refer to include methods such as one-way masking, unspecified air ventilation improvements, and vaccination. However, these protections all have caveats when in settings with higher viral densities, like those occupied by actively shedding and contagious people.
For instance, in regards to masking: A CDC study showed that one-way protection from surgical masks (which are commonly recommended or handed out for use) was only about 56.1% without modifications. Another 2021 study showed medical masks (i.e. surgical masks or procedure masks) without modification blocked approximately 56% of cough aerosols and only 42% of exhaled aerosols (the primary spread of COVID-19 is through aerosols). Even respirator masks, such as N95s, work much better in lower viral densities.
Ventilation and filtration guidelines for infection control also work better in areas with lower viral densities, and these methods will be less effective with active shedders encouraged to attend work and school. Also, CDC did not include specifics needed for ventilation and filtration for the purposes of control of infectious aerosols, especially when the sources of infection are present in the building.
However, the American Society of Heating, Refrigerating and Air-Conditioning Engineers ASHRAE) set Ventilation for Industrial Settings During the COVID-19 Pandemic in 2022, recommending facilities “Maintain between six and twelve air changes per hour (ACH), which will provide a greater than 99% purge in 30-60 minutes.” They note: “This reduction applies when the building is unoccupied – the concept of purging does not apply if a source is still present” (i.e., potentially infectious individuals are still in the space).
In 2023 ASHRAE set Standard 241Control of Infectious Aerosols,which can be previewed here under Standard 241-2023, setting minimum equivalent clean air flow rates for infection risk mitigations for long range transmission according to the building’s occupancy category. For a classroom setting it uses 40 cfm per person, or 20 l/s per persons, which for an average classroom of 25 occupants converts to approximately 8 air changes per hour (ACH)*.
Most schools don't meet even pre-covid minimum ventilation standards, much less the 8 or more ACH they need for infection control.CDC’s last report showed most schools have not upgraded ventilation or filtration. This means at this time the CDC should be trying to reduce the amount of infectious aerosols coming into the classroom, not increase it.
Furthermore, ASHRAE 241 states that its scope“Addresses only indoor long-range transmission resulting from inhalation of infectious aerosol emitted by an infector who is not in close proximity to a susceptible occupant”, further indicating the limitations of ventilation to reduce infection, and that it will not protect people near the contagious person from transmission. At the very least, it is an indicator that people with known or suspected COVID-19 should stay home during the known contagious period of COVID-19, which studies show is between 8 and 14 days in most people. A 2023 study showed a significant amount of infectious virus was detected in the exhaled breath of COVID-positive people for 8 days regardless of vaccination status, and including asymptomatic and mild cases. A person could therefore be infectious longer than the CDC guidelines, even in mild and asymptomatic cases, or cases when symptoms are improving or have stopped.
CDC also states vaccine protection as a reason for policy change, because more people are now protected. They neglect to mention protection wanes over time and offers limited protection from new variants. A recent report shows it is not as protective from infection of newer variants like JN.1, the most prevalent variant in the US at this time. Also, vaccination does not prevent long COVID, which is a significant risk after COVID infection.
A 2022 study published in Nature, found a 15% reduction in long Covid amongst those vaccinated. The authors concluded that “vaccination before infection confers only partial protection in the post-acute phase of the disease; hence, reliance on it as a sole mitigation strategy may not optimally reduce long-term health consequences of SARS-CoV-2 infection.”
A 2023 population-level analysis found vaccines reduced long COVID by 15-20%, with the authors concluding “Complementing vaccination campaigns with potential therapies, as well as further investing on prevention, might reduce the prevalence of long COVID and, consequently, should be considered for public health policies in the next future.”
A 2023 Swedish study analysis found vaccine effectiveness against long COVID was 21% for one dose, 59% for 2 doses, and 73% for 3 or more doses, showing the importance of staying up-to-date on vaccinations, something that is currently lacking in the general population.
Also, vaccine protection is not all or nothing. A 2023 study shows vaccines are muchmore effective in preventing transmission when the person inhales a smaller viral load. Having more contagious people present, and thus more virus in the air, will only increase the amount of virus, or viral load, inhaled.
The CDC states part of its rationale for updating the Infection Control Guidelines is to make it align better with other respiratory infections such as the flu. However, research continues to show COVID-19 is not like the flu. It poses much higher risks in both its acute infection state as well as in its long-term risks. It also has a higher rate of transmissibility, greater ease at getting into cells throughout the body causing system-wide damage, does not have a season but instead poses a threat year-round, is better at evading prior immunity, and it poses higher risks with every reinfection– all of which makes it different than other viruses we know of.
The World Health Network recommends a minimum 14 day isolation period, as the gold standard for isolation necessary for infection control from COVID-19. This recommendation is supported by growing bodies of research.
For instance, a 2022 study showed that, among the SARS-CoV-2 Omicron variant infected patients, viral shedding continues for more than 10 days in 13.5% of all cases, and 11% in symptom-free cases– which means isolation should not be stopped based on symptoms reducing it stopping, and should be continued at least for 10 days.
Researchers further showed that determining infectiousness by symptoms is not accurate: “In 19% of the cases, the duration of shedding was longer than the duration of the symptoms. On day 5, four patients declared no more symptoms, although viruses were isolated by the culture. The rate of viral shedding among symptom-free cases was 58% on day 7, whereas they were 11% on day 10 and 5% on day 14”, showinginfectious virus shedding continued up to 2 days after symptom resolution.
The CDC’s March 2024 updated Isolation Guidance is not the first time they made changes that were not supported by research, but it is the worst. For example, there has not been a reduction in contagiousness of COVID-19 variants over time, but the CDC has modified its isolation standards from its 2020 14-day minimum, to a 10-day minimum in 2022. In 2023, they further modified a 10-day isolation minimum in 2023 to a 5-day minimum, with a mishmash of confusing contingencies, such as increasing that time based on a person's symptoms, their oxygen saturation, their underlying diseases, their ability to avoid vulnerable people, their immunocompetency level, the results of testing, testing type, and consultation visits.
The guidance stated: those with asymptomatic or mild cases (as defined by symptoms and oxygen saturation level) are recommended 5 days isolation followed by 5 days of masking; A 10-day period is recommended for moderate or severe cases; Those with severe COVID-19 may remain infectious beyond 10 days and may need to extend isolation for up to 20 days. People who are moderately or severely immunocompromised should isolate through at least day 20, as well as serial test and consult with an infectious disease specialist prior to ending isolation. And a 10-day minimum is recommended for anyone before being around a person who is at higher risk of severe disease. They stated that these recommendations do not changeeven if you have no symptomsand that these recommendations do not change based on COVID-19 hospitalization levels.
Although the former CDC recommendations were closer to the research than current recommendations, a 14-day gold standard for isolation remains to be aligned with the current research on both contagiousness and within the correct context of severity, including both acute and long-term effects of COVID-19 on the general public. The newer CDC guidelines have taken a step further from the science instead of closer to it.
You can view WHN Isolation and Exit Time guidelines in detail here. We, along with other groups, are pushing back against CDCs reduced isolation guidance, and advocating for 14 day minimum isolation standard.
*8 ACH was found by taking the 40 cfm per person ASHRAE Standard 241 recommendation for classrooms and multiplying it by 20 people to get 800 cfm, and then putting that into a CFM to ACH converter to see that in a 25’x25’x9’ classroom size with 800 cfm would reach 8.5 ACH.
Presentation at 2023 clean indoor air expo
Using Clear Public Health Messaging to Break Barriers to Infection Prevention
by Shea O'Neil
October 2023
The Urgent Need for Clear Public Health Messaging
One of the biggest roadblocks to the goal of reducing infections, slowing viral evolution, and subsequently reducing chronic disease, disability, healthcare strain, premature deaths, and economic blights (i.e. short-term costs, hospitalization costs, long COVID costs, and mortality costs) has been the confusing and often conflicting public health messaging on how to use the tools effectively to prevent COVID-19 infection.
Figure 1: Clear Messaging
There is currently a scientific consensus [1] that one of the most significant modes of transmission for SARS-CoV-2 is through aerosols generated when we breathe and talk.
[1] Scientific Consensus: Aerosol spread has been acknowledged by both the WHO and the CDC. The CDC published a study demonstrating “the high transmissibility of Omicron variants… even across rooms and floors” in a hotel. Since then many studies have been done confirming aerosol-spread COVID-19, including studies on outbreaks and studies using viral genomic sequencing to determine sources, such as a study in which a single patient transmitted SARS-CoV-2 to six healthcare workers (HCW) who were wearing surgical masks (which are made for protection from droplets), as opposed to N95 respirators (made for aerosol protection) as well as spreading it to three other patients. This study noted all the HCWs also wore eye protection and that three of the HCWs had no direct contact and maintained a distance of at least 6 ft from the infected patient. In a real world study on the efficacy of respirator masks in a COVID ward, when surgical masks were replaced with FFP3 (N95) respirators for nurses on a COVID-19 ward, infection risk declined by 52%-100%. A 2021 review of airborne transmission published in Science highlights the number and viral load of aerosols produced through speaking and other expiratory activities are much higher than those of droplets, and they can reach further into the lungs, again affirming aerosols as the primary way COVID-19 is transmitted. A 2021 Lancet analysis of research supporting airborne transmission points out that smaller aerosols showed higher pathogen concentrations than droplets, can linger in the air for hours as well as travel through air conditioner ducts, and that “Reducing airborne transmission of virus requires measures to avoid inhalation of infectious aerosols, including ventilation, air filtration, reducing crowding and time spent indoors, use of masks whenever indoors, attention to mask quality and fit, and higher-grade protection for health-care staff and front-line workers.” According to the US Environmental Protection Agency (EPA): “Transmission of COVID-19 from inhalation of virus in the air can occur at distances greater than six feet. Particles from an infected person can move throughout an entire room or indoor space. The particles can also linger in the air after a person has left the room – they can remain airborne for hours in some cases. Someone can also be exposed via splashes and sprays of respiratory fluids directly onto their mucous membranes. Spread may also sometimes occur through contact with contaminated surfaces, though this route is now considered less likely.”In the 2022 Delphi Consensus published in Nature, a multidisciplinary panel of experts on COVID-19 from across the world contended, “Considering the airborne nature of transmission, governments should regulate and incentivise structural prevention measures, such as ventilation and air filtration, and high priority should be given to preventing SARS-CoV-2 transmission in the workplace, educational institutions and commercial centres.”
Additionally, the dangers of COVID-19 move beyond acute-phase infection, and have, for millions of people, developed into serious, long-term, chronic, disabling, and even deadly effects of long COVID [2].
[2] Long COVID, also referred to as post-acute sequelae of COVID-19 (PASC), has affected millions of people and can cause a wide range of serious complications including disability and death. According to a 2023 Nature article, “long Covid incidence is estimated at 10–30% of non-hospitalized cases, 50–70% of hospitalized cases and 10–12% of vaccinated cases …Symptoms can last for years, and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong. With significant proportions of individuals with long COVID unable to return to work, the scale of newly disabled individuals is contributing to labour shortages. There are currently no validated effective treatments.” A 2021 systematic review found more than half of COVID-19 infections resulted in long COVID six months after recovery. Long COVID can result in long-term cardiovascular outcomes, gastrointestinal problems, multi-organ impairment, abnormalities of blood vessels and coagulation, mitochondrial dysfunction, functional impairment and fatigue, muscle abnormalities, immune dysregulation, detrimental neurological impacts (including brain cell fusion, depressive, and cognitive impacts), and increased risks associated with reinfections. A 2023 Nature immunological review concluded “The oncoming burden of long COVID faced by patients, health-care providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it. If 10% of acute infections lead to persistent symptoms, it could be predicted that ~400 million individuals globally are in need of support for long COVID.” A 2023 Scientific American article stated “the most common, persistent, and disabling symptoms of long COVID are neurological”, later quoting a physician saying, “I now think of COVID as a neurological disease as much as I think of it as a pulmonary disease, and that's definitely true in long COVID.” Although formal guidance on how to record long COVID on death certificates was not released until 2023, CDC data from early 2024 has shown thousands of deaths of US citizens from long COVID. The only way to prevent long COVID is to prevent COVID-19 infection. Persistent infections- those that last longer than 30 days with replicating viruses– have also been implicated in the evolution of new viral variants, suggesting that reducing infections will also slow viral evolution.
Now that we know, we need to develop the appropriate public response and policy-making response [3]. We need to acknowledge where our messaging has gone wrong, where it was politicized, and back away from misinformation, anger, unwillingness, and confusion about the science.
[3] Public health policy response has not been updated in healthcare, workplaces, or schools around the world to align with prevention of aerosol spread viruses. In “Mitigating airborne transmission of SARS”, published in the The Canadian Medical Association Journal, the authors state, “Although good ventilation can mitigate long-range aerosol transmission of SARS-CoV-2, the WHO and CDC’s acknowledgement of airborne spread at close range highlights an urgent need to revisit PPE guidelines in all Canadian health care settings.” They point out that high-quality masks such as N95 respirators are currently required only for “aerosol-generating medical procedures”, despite studies that have shown that “exertional activities and coughing produce more aerosols than some aerosol-generating medical procedures”. They also point out that because SARS-CoV-2 can be spread by both short-range and long-range aerosol inhalation, ventilation needs to be combined with the known guidance that “recognizes that N95 respirators are the gold standard for protection against short-range aerosol inhalation.” They go on to say how these measures are important outside of healthcare settings as well, stating: “Although social measures such as paid sick leave are vital, standardized masks (ideally, fit-tested respirators) are still a critically important protective measure.” In the US, the CDC is currently reviewing infection control guidelines in healthcare, and current drafted guidance, although acknowledging N95 respirator masks provide superior infection, call instead for surgical masks requirements and do not include ventilation or filtration guidelines. Similar concerns have been raised to the NHS regarding updates to the Infection Control Manual in England by the British Medical Association. And, according to a multinational Delphi Consensus to end COVID-19 as a public health threat, a panel of 386 academic, health, non-governmental organization, government and other experts in COVID-19 response from 112 countries and territories were in near-unanimous agreement that “SARS-CoV-2 is an airborne virus that presents the highest risk of transmission in indoor areas with poor ventilation. Risk-related communications from all actors should clearly emphasize that transmission of SARS-CoV-2 is primarily caused by inhalation of the virus.” Furthermore, they stated: “vaccination alone will not end COVID-19 as a public health threat. Infection rates tend to increase when governments discontinue social measures, including non-pharmaceutical interventions, regardless of the level of vaccination. Thus, all countries should adopt a vaccines-plus approach, including a combination of COVID-19 vaccination, other prevention measures, treatment and possibly financial incentives.”
As we have seen at events such as the 2023 Clean Indoor Air Expo, the technologies exist, the impetus exists, and the science and research into COVID-19 transmission and long-term effects of COVID-19 exist. Yet, having the tools available is one thing, and getting people to use them effectively is another. This can be helped with clear public health messaging.
Reducing Infections with Clear Public Health Messaging
Two properties about protections from infectious diseases are important:
(1) Defining individual and societal responsibilities, and
(2) Describing the type, level, and combinations of protections needed to effectively to prevent infections.
Let’s take a closer look at how we can use clear public health messaging for each of these properties to reduce transmission.
Shared Individual and Societal Responsibilities
The responsibilities of implementing protections from communicable diseases are shared between individuals and societies, and cannot be assessed as an individual responsibility alone. This is because the decision of one individual to engage with risk may limit the ability of other individuals to protect themselves. When risk is shared, mitigation efforts require collective action to succeed. Typically, the more society does to mitigate a risk, the less of the burden falls onto the individual. However, neither of these entities can be successful acting alone. This notion runs contrary to the "You do you" approach that has become popular amongst public health agencies, that places the burdens and responsibilities solely on individuals.
Figure 2: Shared Individual and Societal Responsibilities

Water safety is a good example of how society manages collective responsibility for a shared risk. How well a government develops and implements water safety standards, how well municipalities monitor and test water, how well responders report incidences of contamination, are all important factors impacting how effectively an individual is able to protect themselves. The individual is responsible for responding to messaging to disinfect or avoid the tap water when directed, as well as to take everyday precautions when handling water to reduce contamination risks.
No lone entity can maintain the full burden of responsibility for shared risks. When it comes to COVID-19, both individuals and groups in society need to be aware of the risk that exists, how the protections work, why they are necessary, and why widespread participation provides the best chance at success to effectively prevent transmission and infection. Part of this is understanding how the layers of protection actually work, and incorporating both the combination of layers as well as the level, or strength, of each layer to use them successfully.
What are the Layers of Protection?
In this paper, we talk about protections in terms of “layers” and “levels”. The layers of protection are the actions that can be taken to prevent the spread of disease from an infected individual to someone without an infection. For a disease like COVID-19 that transmits through the air, these layers include:
Having households avoid being with other households in the same spaces, i.e. homes, schools, workspaces. Protection: Remote (ie virtual options, curbside pickups, delivery)
If people need to be together, then the space itself has to be safe for people to be together. Protections: Masking, physical distancing, air filtering, ventilation, symptom screening, properly testing, properly isolating.
Finally, as a backup, we can help people who are infected better protect themselves biologically from the effects of the infection. Protections: Vaccination, treatments
Let’s take a look at some models to see how these layers of protections work together in different ways to reduce infection and transmission risks.
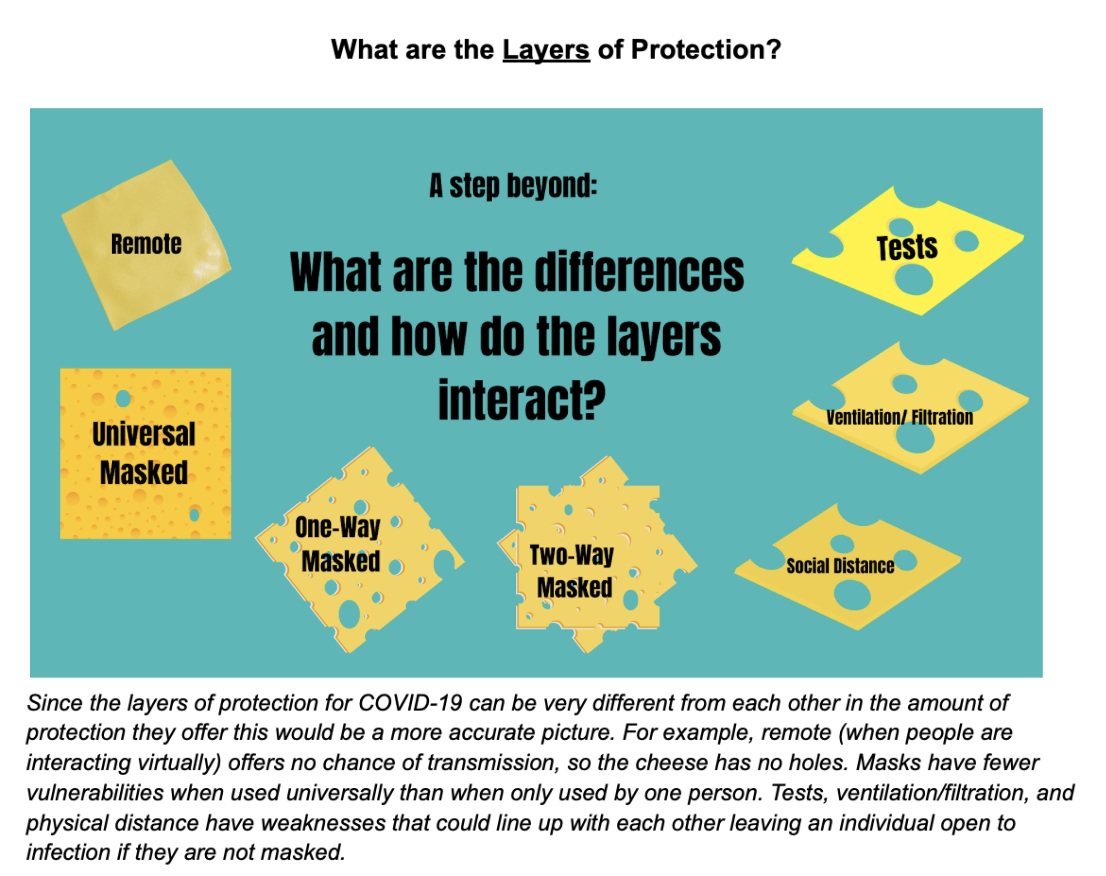
The Need to Move Beyond the Swiss Cheese Model
The Swiss Cheese Model is a popular way to describe a multi-layered approach to COVID-19 prevention. In this model each protection, or layer of prevention, constitutes one piece of swiss cheese, and its weaknesses are represented as the holes. We can stack the slices of cheese (preventions) to reduce the chances that something (COVID-19) makes it through the holes (exposure leading to infection).
Yet, the Swiss Cheese Model has two important limitations. First, it fails to account for the differences in the amount of protection each layer offers. It also ignores how each layer’s strengths and weaknesses interact when combined with other layers.
Figure 3: Weaknesses in Using the Swiss Cheese Model
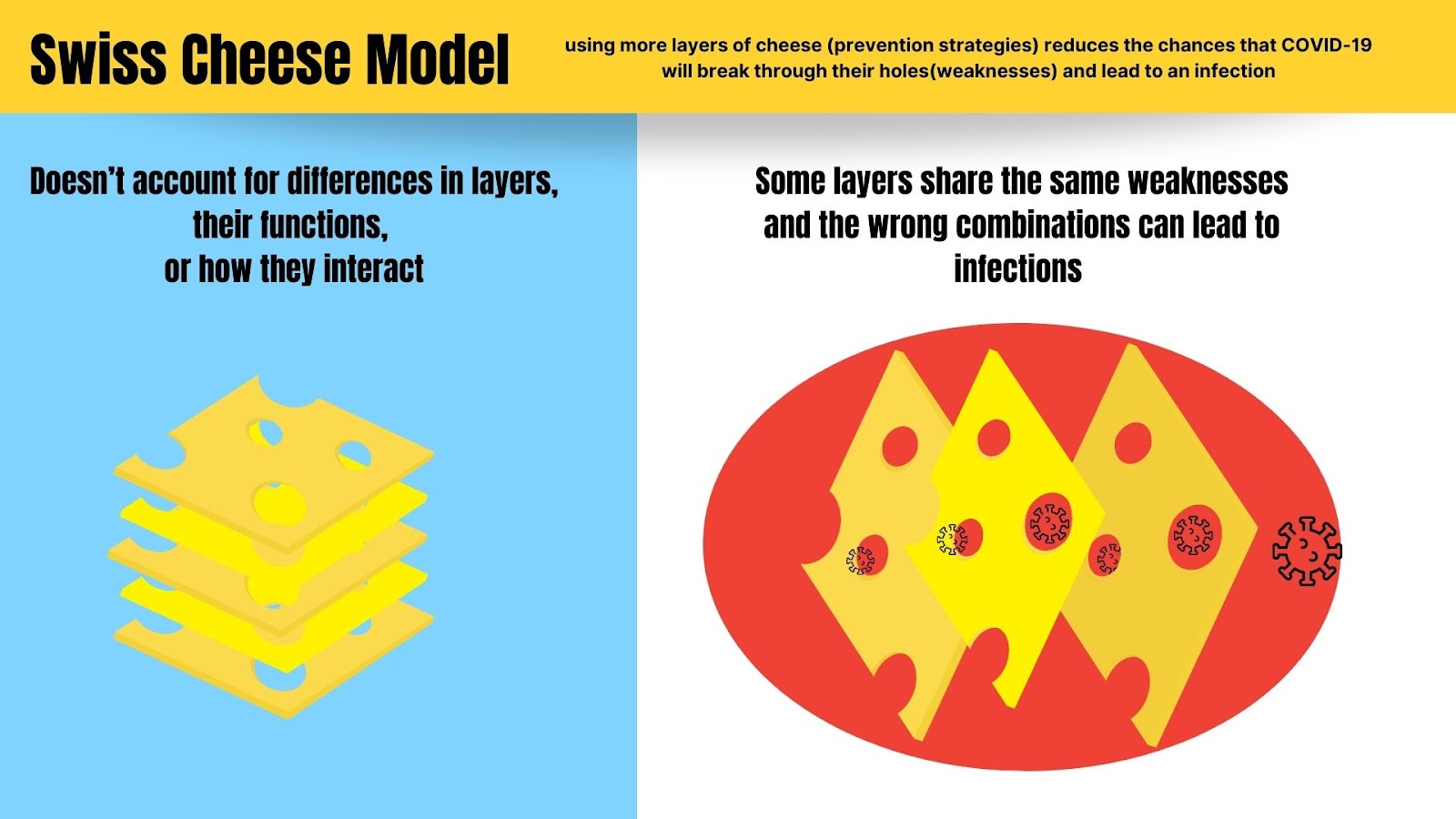
Figure 3 Description: In the Swiss Cheese Model, the layers of protection for COVID-19 are all viewed as having the same amount of holes (weaknesses). It does not describe how the holes (weaknesses in layers) might line up in certain combinations and lead to infections.
For instance, if the slice of cheese representing masks has the fewest holes and we remove it from the stack, our remaining slices (let’s say, air filtration and testing) could have holes that line up, and therefore let through an infection. This is because tests and air filtration have limitations that other protections like masks do not. Testing with a Rapid Antigen Test can lead to false negatives in many cases, sometimes nearly half, allowing an infectious person to enter a space. Air filtration takes time to clear the air and does not prevent an infectious dose of the virus from moving through the air from one person to another while they are talking without masks on. Those layers at those levels do not protect adequately.
Figure 4: A More Accurate Portrayal of the Differences in Layers
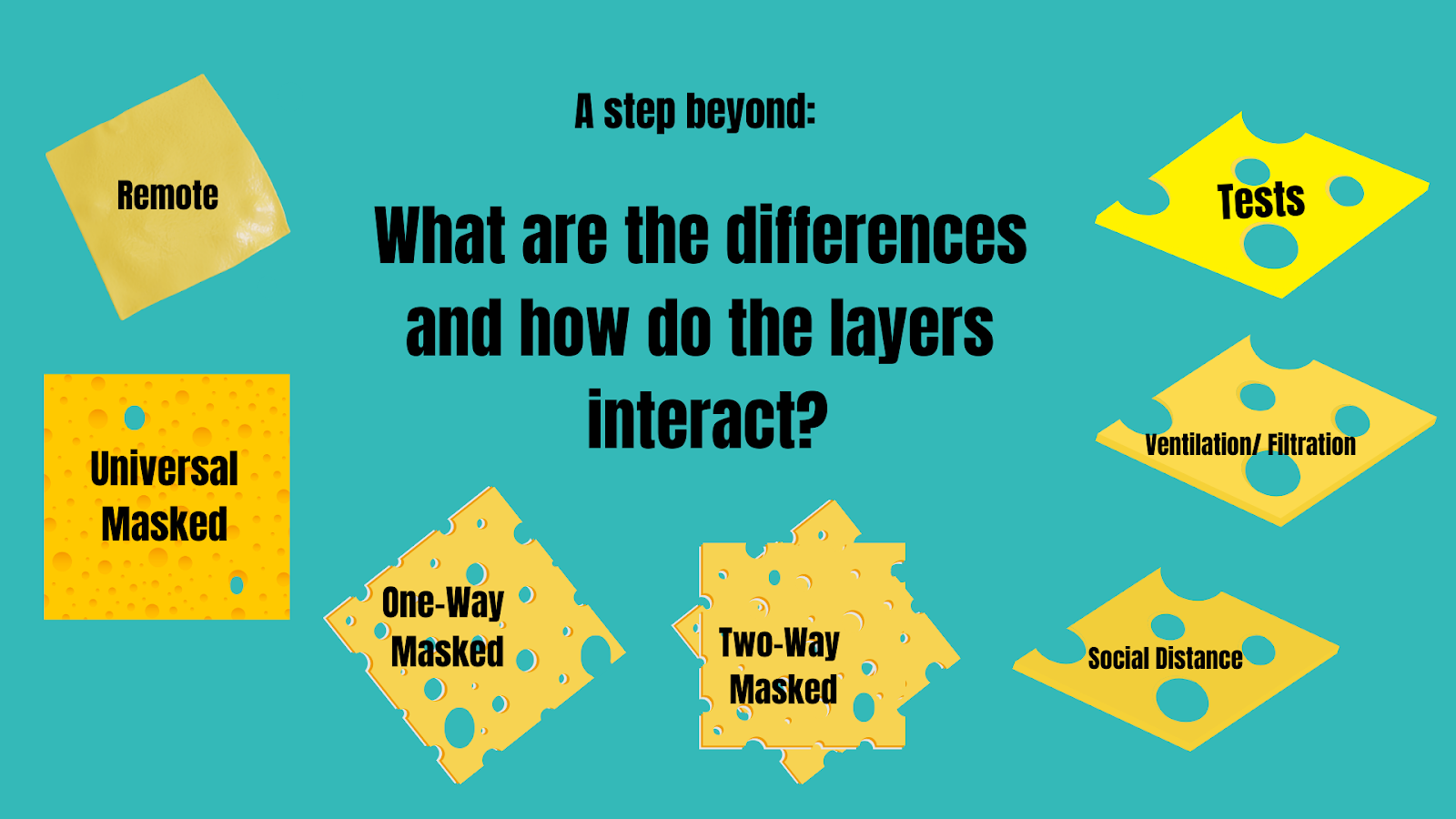
Image Description: Since the layers of protection for COVID-19 can be very different from each other in the amount of protection they offer, Figure 4 above would be a more accurate picture. For example, remote (when people are interacting virtually from their home environments) offers no chance of transmission, so the cheese has no holes. Masks have fewer vulnerabilities when used universally than when only used by one person. Tests, ventilation/filtration, and social (aka physical) distance have weaknesses that could line up with each other leaving an individual open to infection if they are not masked.
Clear public health messaging needs to communicate how we can use different layers, different levels of the layers, and correct combinations of the layers to provide protection from infection.
What are the Levels of Layers?
It is important to recognize that each of the layers also can be applied at different levels, and those levels offer different degrees of protection. The 5 Pillars of Protection model gives three levels for all but one of the layers, which it conceptualizes as pillars rather than slices of cheese.
The 5 pillars and their levels include:
Masking
Level 1: N95,
Level 2: P100 Respirator,
Level 3: PAPR
2. Air Quality
Level 1: 6 ACH (Air Changes per Hour),
Level 2: 12 ACH,
Level 3: Analyzing Air flow
3. Social/ Physical Distancing/ Remote
Level 1: Maximize physical space between people
Level 2: Hybrid Remote,
Level 3: Fully Remote
4. Testing
Level 1: Twice weekly testing with RAT or NAAT;
Level 2: Daily testing with NAAT;
Level 3: Twice daily with NAAT
5. Vaccination: up-to-date
Figure 5: The 5 Pillars of Protection
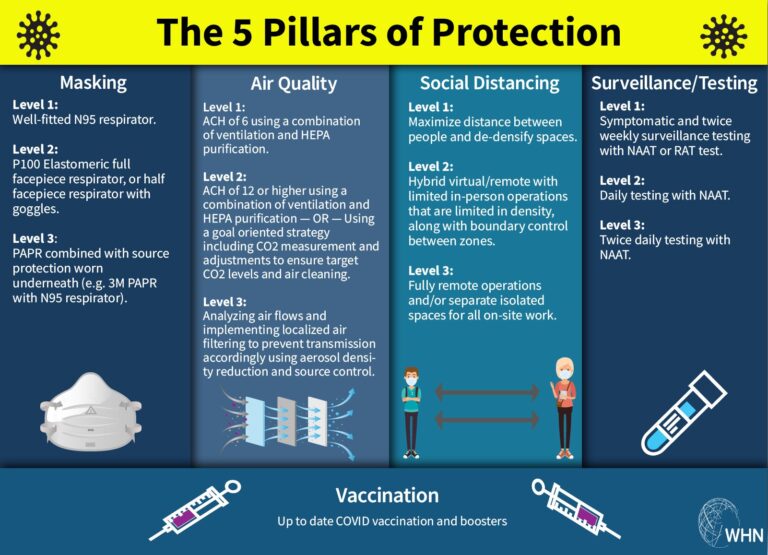
Image Reference: The Five Pillars of Protection and their levels, by the World Health Network
The concept of the 5 Pillar model is that if there is a weakness in one pillar (or layer), increasing the levels of other pillars will help accommodate for the weakness. For instance, if you were in a setting with air quality at less than level 1 (which is 6 ACH), you could raise the levels of other layers (i.e. increase masking level from N95 to a P100 elastomeric; increase physical distancing to hybrid virtual options; increase testing to daily testing with NAAT.) A weakness in the model is that it does not define how to find correct layers, levels, and combinations that work to reduce infections.
Masking: An Essential Layer
As stated earlier, not all layers of protections are equal in the amount of protection they provide, and none of the layers is sufficient on its own. One of the first layers many people try to drop when using a multi-layered approach is a respirator mask.
However,
Most other layers of protection are not sufficient on their own to prevent infections, and need to be used in combination with masks to best reduce infection risks. Respirators, such as N95 masks and further described in this work as “masks”, offer source control that is unachievable by other means. Masks can directly filter the air as it is exhaled from a possible source (when the source is masked), and again before you breathe it in (when you are masked) thereby significantly reducing transmission of infectious aerosols, including COVID-19 [4].
[4] Masks work: A pre-COVID study showed respirator masks significantly reduced infections with airborne pathogens, also showing continuous use of respirators to be more effective than intermittent use. A 2021 report published in Science concludes facemasks effectively limit the probability of SARS CoV-2 transmission, while also acknowledging that mask efficacy depends on airborne viral load, adequate fit and filtration, and is increased with using other protections to reduce viral load. As mentioned earlier, in a real world study on the efficacy of respirator masks in a COVID ward, when surgical masks were replaced with FFP3 (N95) respirators for nurses on a COVID-19 ward, infection risk declined by 52%-100%. A study published in PNAS showed with only the susceptible wearing a surgical mask, the upper bound of infection risk is 90% after 30 minutes. However, when both the susceptible and infected wear a well-fitted respirator mask, the risk is 0.4% after an hour. A 2022 research article titled “Mask wearing in community settings reduces SARS-CoV-2 transmission” found that the mean observed level of mask wearing corresponded to a 19% decrease in the reproduction number, and stated that “the evidence that mass mask wearing reduces transmission implies that mandates (and other mask-promotion policies) may be effective against COVID-19 if and when they improve or increase the use of masks.” A 2021 study showed universal masking is significantly better than one-way masking. A 2022 study published in the Journal of Infectious Diseases found that fit-tested N95 mask combined with a portable HEPA filtration system offers the best protection against viral particles in the air.
Because studies show that much of SARS-CoV-2 transmission is from asymptomatic or presymptomatic carriers, it is important to mask when around others outside your household, whether you/they are experiencing symptoms or not [5].
[5] Asymptomatic and Symptomatic Transmission of COVID-19: According to a 2023 study, transmission can happen in as little time as 20 seconds to 4 minutes (depending on whether it's a high shedder or average shedder), and high levels of infectious virus were detected in exhaled breath regardless of vaccination status, with significant amounts emitted even in mild and asymptomatic cases. A Nature study from December 2023 also showed transmission can happen in as little as a few minutes in normal indoor environments. A 2022 systematic review on transmission concluded: “High-quality studies provide probable evidence of SARS-CoV-2 transmission from presymptomatic and asymptomatic individuals.” A 2021 study using data from infector-infectee pairs found high infectiousness immediately prior to symptom onset. And, in a study published in JAMA in 2021, an analytical model found transmission from asymptomatic individuals was estimated to account for more than half of all transmissions.
When wouldn't Masking be prescribed?
While you are working remote/ virtual from your home
For children under the age of two (24 months)
For those who have certain disabilities, who are unable to safely wear a mask due to that disability.
For those who are in medical situations in which it is medically contraindicated to wear a respirator mask.
Finding the Respirator Mask that Works Best For Your Situation
You should try out different kinds of respirators such as N95 masks to find the best fit and comfort. There are many masks that allow for greater breathability, have see-through windows, are latex-free, and come in a variety of sizes and styles. Environment, activity level, and time can also be modified to find compatible adaptations. There are also N95 masks without metal in them for use in certain medical situations.
Figure 6: Respirator Masks, Like People, Come in Many Shapes and Sizes
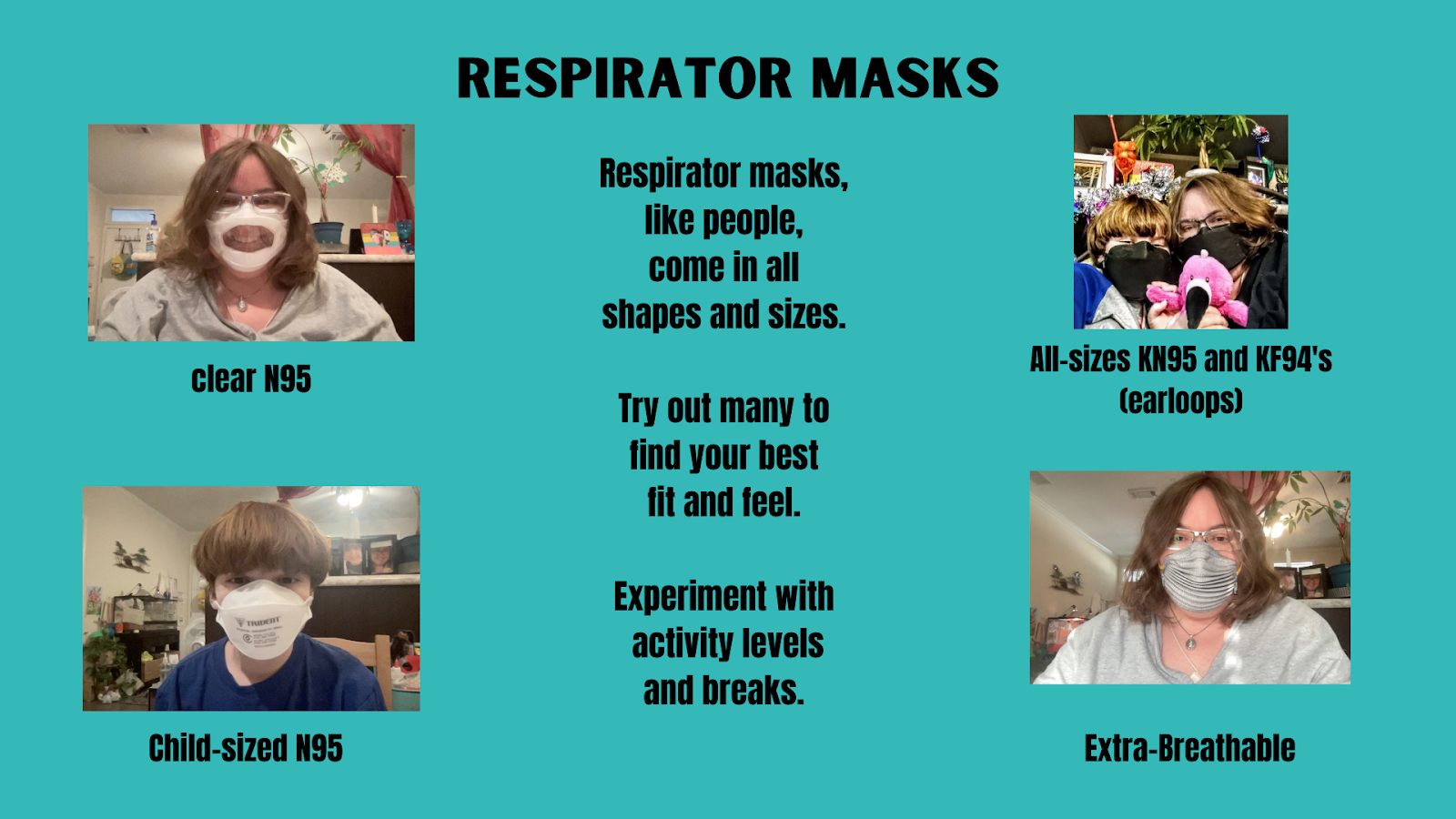
Figure Description: There are clear N95 masks for those who need to see mouths (top left photo), child-sized masks for children 2 and above (bottom left photo), KF94 with adjustable ear loops for adults and children (top right photo), N95 masks with folds that increase airflow for adults (bottom right, adult size pictured) and smaller sizes for adults with small faces and children (not pictured, but same design).
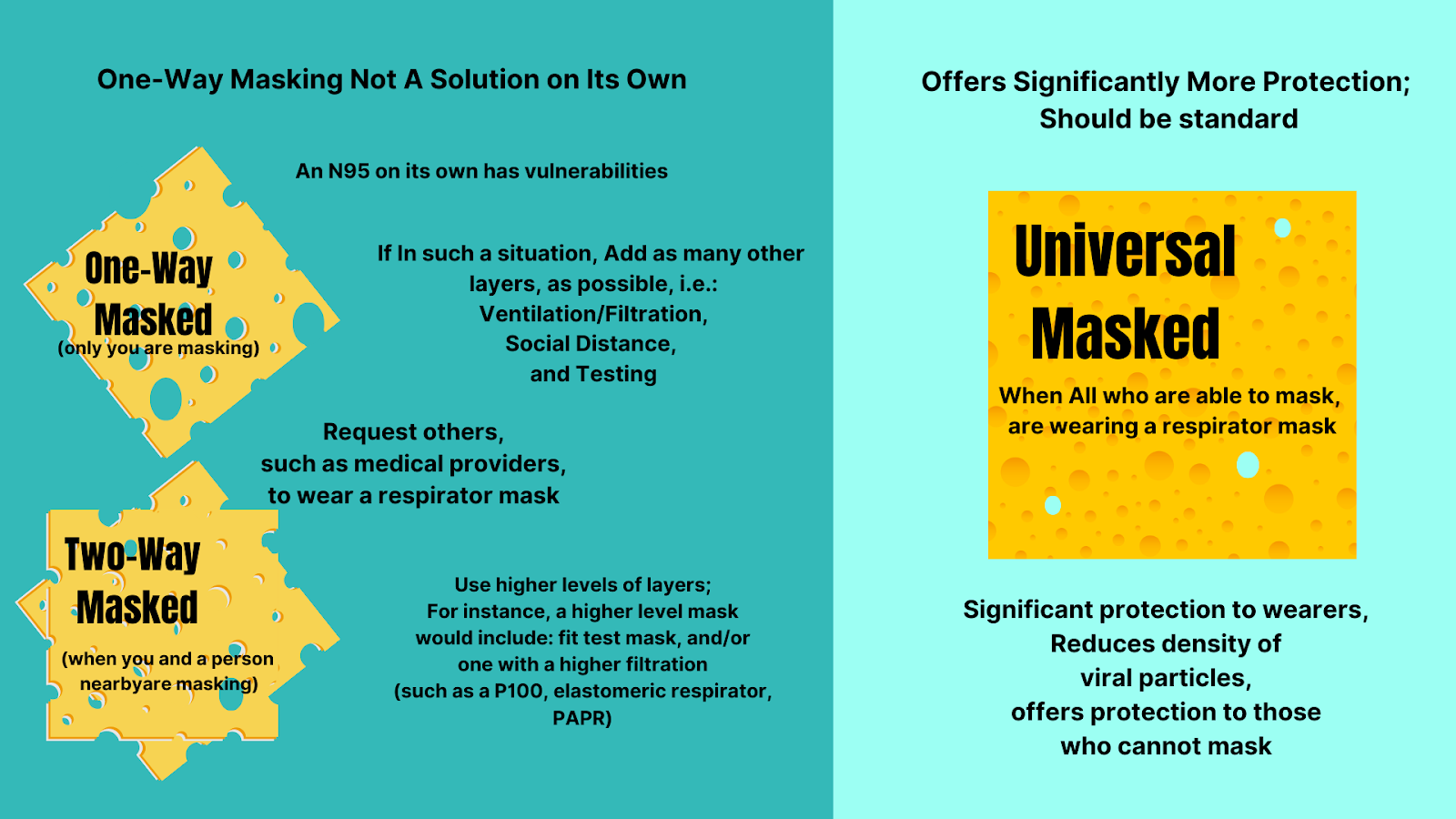
Is Masking an Individual Responsibility or a Collective Responsibility?
Masking is both an individual and collective responsibility because COVID-19 is a shared risk. When you have individuals in society who cannot mask (infants, those with certain disabilities or medical conditions), it is even more important that those around them ARE wearing a respirator mask, alongside other layers of protection. The more people who are masking in a space, the lower the risks of COVID-19 transmission, and the more protection offered to all– including those who cannot wear a mask.
It is also worth noting that one-way masking offers very limited protection, regardless of your individual risk profile. Universal masking offers significantly more protection than other masking situations.
One-way masking (when you are the only one masked) will require more layers of protection and/or higher levels of protection than two-way masking (when you and a person nearby are masking) or in universal masking (when all are masking) situations. If you find yourself in an unavoidable non-universal masking situation, you will want to take additional precautions. For example, you can improve your mask’s efficiency by finding one with a better fit, or with a higher level of filtration, (examples: fit-tested N95, elastomeric respirators, and PAPRs). You can also ask for others, such as medical providers and those interacting with you, to mask with N95s and use other reasonable accommodations to reduce exposure.
Figure 7: The Differences Between One-Way, Two-Way, and Universal Masking
Using Supporting Layers to Create Safe Shared Spaces
Shared spaces are any spaces where multiple households come together. They include public spaces such as schools, libraries, post offices, city centers, courthouses, etc. They also include private businesses and homes when multiple households gather there. Outdoor venues are considered shared spaces, since COVID-19 can spread outdoors (although outdoors does have an advantage of the layer of good ventilation, it is also affected by other factors such as the density of people in that space).
Shared spaces can be made safe by a combination of 2 factors:
1- reducing the amount of virus coming into a space, and
2- filtering the remaining virus out before it is breathed in by people in that space.
Figure 8: Reducing Viruses Coming In, Filtering Out Viruses That Do Get In
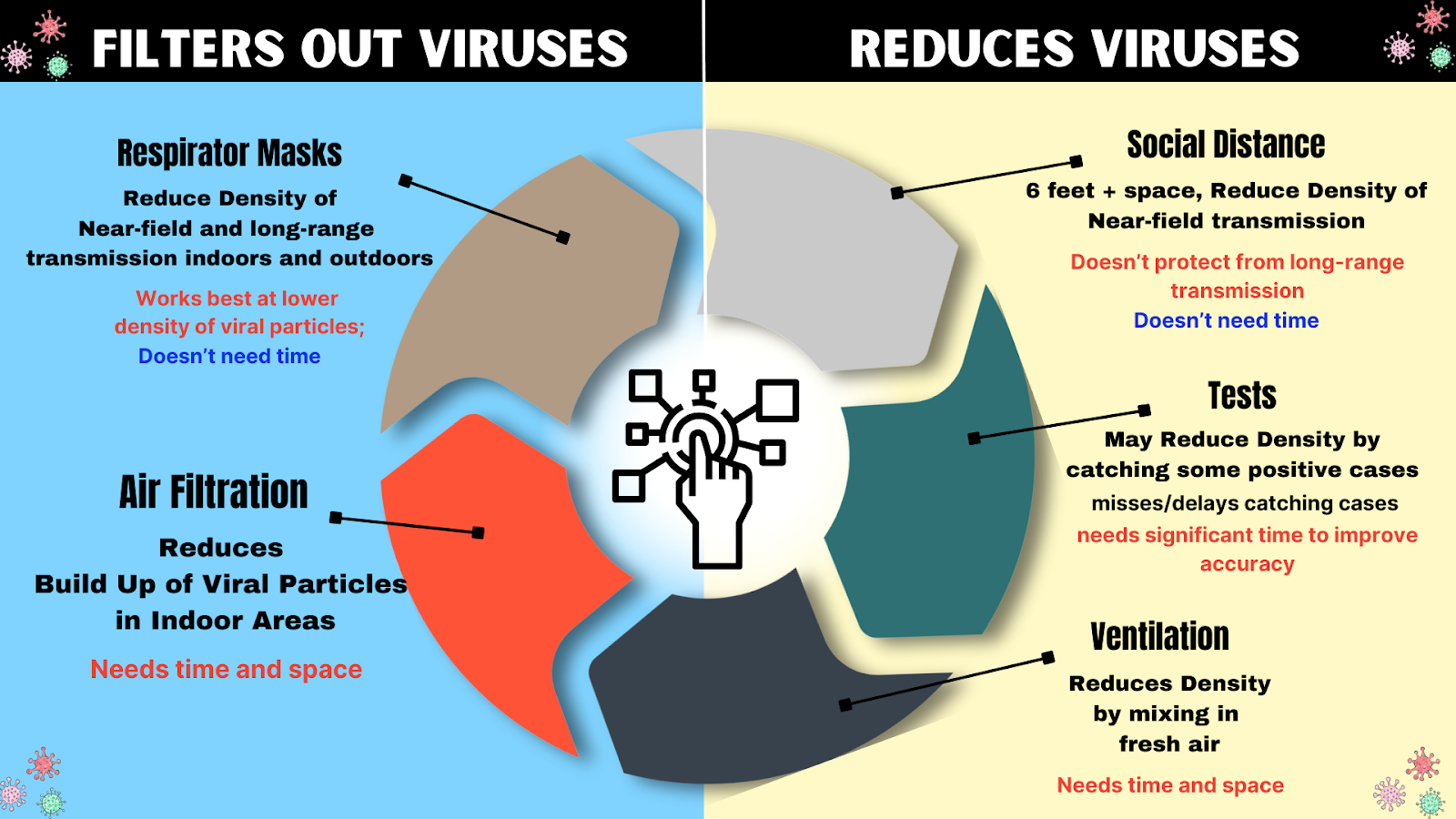
The combinations of certain layers of protection help to account for others’ weaknesses. For instance, masks work better at lower density of particles. Since viral particles are higher near the source, physical distance from the source can lower viral density, and thus compliment masks.
Air filtration and ventilation reduce long range transmission, but, because they require time and space to clear out the virus, they have a gap in protection that a mask can fill with its immediate protection.
Testing will reduce the chances of an infectious person coming into a space, but because tests require multiple tests over the course of days to provide accurate results and miss positive cases, in most cases they can only be used to reduce some viral load, again needing other layers to fill in the gaps in protection from missed cases, such as masking and filtering the air.
Protections such as social/physical distance, testing, and ventilation reduce the amount of virus coming into a space. Protections such as masking and air filtration filter out viruses. Both are important and complementary methods of reducing infection risks.
Supporting Layer: Adequate Ventilation and Filtration
Enhanced ventilation and filtration to the 6-12 Air Changes per Hour (ACH) range, in addition to masking, is recommended for the purposes of infection control, leaning towards the higher end when higher numbers of people are present in the space. Viruses like COVID-19 that can spread through aerosols can travel far through the air, remain infectious for hours, and transmit illness to others. Such infections can be greatly reduced by adding enhanced ventilation and filtration [6].
[6] Enhanced Ventilation/Filtration: In a 2022 bioaerosol study on the infectivity of coronaviruses, researchers explained that saliva acted as a protective mechanism for the virus. They found at both 40% and 60% relative humidity, half of the airborne coronavirus particles were still infectious after aging for one hour, and that at 25% humidity, half of the original particles remained infectious for two hours. A 2023 study published in Nature researchers' data showed that “exhaled aerosols from a single person can transmit COVID-19 to others within minutes at normal indoor conditions.” A 2022 study published in the Journal of Infectious Diseases showed when combined with fit-tested N95 masks, gloves, and face shields, HEPA filtration provides protection against high viral loads over prolonged periods of time by reducing virus to near-zero levels. A 2022 systematic review of 11 studies also found HEPA purifiers significantly reduce airborne SARS-CoV-2 viral aerosols. HEPA purifiers and fan and Filter air cleaners such as the highly effective Corsi-Rosenthal Box (CR-box) have been shown to remove infectious particles and are recommended by CDC and NIOSH for reducing COVID-19. A 2022 study found using HEPA filters to the 7-12 air changes per hour can consistently remove SARS-CoV-2 and reduce viral load to below the detection limit, noting that because air does not pass through the air cleaner evenly, that it does require time, and that there are areas where the aerosols tend to linger, it should be combined with other measures. In a 2022 study researchers state: “Our analysis shows that mitigation measures to limit shared-room airborne transmission are needed in most indoor spaces whenever COVID-19 is spreading in a community. Among effective measures are reducing vocalization, avoiding intense physical activities, shortening the duration of occupancy, reducing the number of occupants, wearing high-quality well-fitting masks, increasing ventilation, improving ventilation effectiveness, and applying additional virus removal measures (such as HEPA filtration and UVGI disinfection). The use of multiple “layers of protection” is needed in many situations, while a single measure (e.g., masking) may not be able to reduce risk to low levels.”
In homes, ventilation and filtration is an individual responsibility. In public spaces it is a societal responsibility (although, in the absence of enhanced filtration or ventilation in a public space, individuals can attempt to compensate by bringing their own air purifiers).
Proper ventilation and/or filtration can be achieved by combining HEPA purifiers, CR box-style fan/filters, installing MERV 13 filters into HVAC systems, using mechanical ventilation, and/or opening windows. Tools such as Clean Air Stars, Rochester CADR Calculator, Smart Air CADR/ACH Calculator, or OHCOW Ventilation Calculation Tool are helpful in determining the type and number of purifiers to reach the appropriate air changes per hour for your space.
ASHRAE (American Society of Heating, Refrigerating and Air-Conditioning Engineers) has released standards for control of infectious aerosols in both 2021 and 2023. In ASHRAE Standard 241 (2023), it sets standards for the equivalent clean air flow rate, or the flow rate of pathogen free air into occupied areas of different settings that would have the same effect as the total of outdoor air needed to substantially reduce the amount of disease transmission in different settings [7].
[7] ASHRAE Standards: ASHRAE’s 2021 Ventilation for Industrial Settings During the COVID-19 Pandemic states: “Maintain between six and twelve air changes per hour (ACH), which will provide a greater than 99% purge in 30-60 minutes. This reduction applies when the building is unoccupied – the concept of purging does not apply if a source is still present (i.e., potentially infectious individuals are still in the workspace). It is important to maintain as much outside air and/or sufficiently filtered recirculated air as possible to achieve the goal of > 6 ACH.” The 2023 ASHRAE Standard 241Control of Infectious Aerosols, which can be previewed here, sets minimum equivalent clean air flow rates for infection risk mitigations for long range transmission according to the building’s occupancy category. In Table 5-1 they define spaces such as gym, classroom, lecture hall, classroom, health exam room, residential common space, etc and expresses the minimum equivalent clean airflow rate required using cubic feet per minute (cfm) per person as well as liter per second (l/s) per person to allow for better variation based on number of people in the room and activity level of the people. For a classroom setting it uses 40 cfm per person, or 20 l/s per persons, which for an average classroom of 25 it converts to approximately 8-12 ACH.
Ventilation and filtration need space and time to clear viruses out of the air. Masks give you protection in that space and time, while ventilation and filtration lower the density of infectious particles, making masks more effective.
One can use directed air flow, or blowing clean air (such as that from a handheld HEPA purifier) into your breathing space, to reduce chances of viral particles being in the vicinity. This can be especially important in situations where masking cannot be done, such as by a patient receiving dental work (for more information, see WHN’s Dental Safety Guide).
Supporting Layer: Social (Physical) Distancing
Social distancing, that is physically distancing people 6-10 feet apart, works as a supporting layer when combined with other layers, but does little on its own [8].
For one-way masking, personal space (6 feet) becomes even more important, as exhaled aerosol density is stronger closer to the source, and masks work better at lower viral density.
Physical distancing provides the space and time necessary for ventilation and filtration to start to clear infectious particles out.
Note: 6 feet is not a magic number. Infectious viral aerosols can and will travel beyond this distance, which is why wearing a mask is necessary even when spaced out.
[8] Physical Distancing: A 2021 study that looked at the combination of layers as opposed to each one singly, concluded that “Increases in ventilation rates, the use of HEPA air cleaners, the implementation of universal masking, and physical distancing can all play a role in decreasing the exposure of room occupants to airborne SARS-CoV-2. In this investigation, universal masking was the most consistent and efficacious mitigation strategy. Masking (the study used 3-ply surgical masks) reduced exposure by 50% or more compared to no masking. Ventilation reduced exposure by approximately 5% per 1 ACH increase, irrespective of whether increasing ventilation was achieved by increasing system HVAC or by the use of portable HEPA air cleaners. The placement of portable HEPA air cleaners was a factor in determining a Recipient’s exposure reduction. Nonetheless, the most effective portable HEPA air cleaner configuration was the use of two units at opposing sides of the room, e.g., one at the front and one at the back or one each at the sides of the room, or two units in the center of the room. Increasing physical distance between the Source and Recipients beyond 0.9 m provided minimal exposure reduction when oriented side-by-side. However, maintaining a physical distance of 1.8 m or more between the Source and a Recipient in the face-to-face orientation was critical”. A 2021 article published in the ASHRAE Journal discussed their modeling study with mannequins made to “inhale” and “exhale” aerosols in a modified classroom layout (7 feet separation between students and a 10 foot buffer separation between the instructor and seated students) found that exhaled aerosol density is stronger closer to the source, and that while evaluating various types of masks designed to cover the nose and mouth with the intent of providing protection for the wearer (inhalation) and for those in physical proximity to the wearer (exhalation), mask fitters or braces better enabled the mask to achieve full filtration potential consistently by reducing air leakage around the mask. Another 2021 study published in Science found that “effective ventilation and social distancing will reduce ambient virus concentrations and increase the effectiveness of face masks in containing the virus transmission”.
Remote and Virtual Options
Remote and virtual options are the highest level of physical distance, and, when you are in different physical environments from other households, you do not need to use other layers of protection. Although not all activities can be done remotely, increasing remote activities will reduce overall risks. Places that add remote options provide access and protection to those seeking such options, providing benefits to employees, patrons, and society as a whole.
Remote and Virtual options are becoming increasingly available, with use of online video platforms such as Zoom, Google Meet, and Slack allowing people to interact from any location.
Virtual schools, work from home jobs, telehealth, mobile care services, online ordering/delivery, and curbside pickup options are ways to reduce risks and exposures to COVID-19.
Hybrid options and flexibilities, also encourage better adherence to proper isolation guidance for people who are feeling ill, testing positive, and/or were recently exposed to COVID-19 by allowing them to work from home in those situations reducing impacts of absences on both the individual and group.
Individuals can choose to use remote options as alternatives to attending shared in-person spaces that are not implementing protections. This will not only keep them safe but will encourage those in charge of physical spaces to take the steps needed to make their spaces safer by using the above protections.
Supporting Layers: Testing And Isolating
Testing
Testing [9] can be used to screen for and pick up COVID-19 infections with varying degrees of accuracy depending on:
When the test is taken: Recent data shows viral loads peak on the fourth day after infection. Therefore, it is important to continue testing after exposure for at least four days, as earlier tests may miss picking up infections;
How often one tests: Accuracy improves with serial testing. The FDA recommends repeat testing at least 3 times at 48-hour intervals when asymptomatic, and 2 times separated by 48 hours when symptomatic;
Type of test taken: Molecular tests, such as polymerase chain reaction (PCR) tests are more accurate than Rapid Antigen Tests (RATs); Home molecular test kits are available (Lucira COVID, Lucira COVID+flu, or Metrix COVID test kits), which detect viral genetic material like PCR tests. These home molecular tests are more sensitive and accurate than antigen tests, but they are also more expensive (some are $25-50 per test or require the one-time purchase of an expensive reader);
Symptoms: Tests are more likely to pick up symptomatic cases than asymptomatic cases. (Note: Both asymptomatic and symptomatic people can be infectious).
How the sample is collected: Viral loads tend to rise in the throat before the nose, and collecting both nose and throat samples can significantly improve accuracy.
The age of the person: children and young adults have lower accuracy ratings than adults in some studies.
Other factors: type of comparator a test brand uses (BinaxNow comparator was not as accurate for Omicron than it was for Delta); timing of last vaccine or infection.
Catching COVID-19 on a test at onset has proven extremely difficult since many people are either pre-symptomatic or asymptomatic. The tests have worse accuracy with asymptomatic and presymptomatic infections despite the person being contagious.
Testing is valuable because identifying infections can assist with getting timely treatment as well as motivating people to isolate for the correct amount of time and therefore reducing transmissions. It is also good to confirm infections in case one develops long COVID later on.
However, because tests can miss and/or delay picking up many cases, they cannot rule out an infection or contagiousness. For this reason, masking should not be removed unless a regimen is followed to have that person enter your "bubble", which often requires quarantine isolation periods, and multiple tests, as symptoms may appear 2-14 days after exposure.
[9] Testing Accuracy/Infectiousness: Studies have found: ~63% of people don’t have symptoms when they are first infectious with the Omicron variant, and ~32% don’t ever develop symptoms even though they can infect others. According to a 2021 study in the Journal of Infectious Diseases, PCR tests are more accurate than RAT tests at both picking up asymptomatic or presymptomatic individuals before they can transmit the virus, thus mitigating spread, as well as identifying individuals at later stages of infection. They noted both test types should be done serially, at least every 3 days. A 2023 study on the performance of rapid antigen tests found accuracy was optimized when asymptomatic participants tested 3 times at 48-hour intervals and when symptomatic participants tested 2 times separated by 48 hours. Tests are more likely to pick up symptomatic cases than asymptomatic cases. In a 2022 study on the accuracy of RAT tests with Omicron variants in students ages 17-22 found that among symptomatic participants, RAT had a sensitivity of 77.8%; among asymptomatic patients, accuracy was only 39.2%. A 2023 study shows collecting both throat and nasal samples improved RAT accuracy by 15-21 percentage points, as Omicron viral loads rise in the throat before the nose. A2021 cohort study published in JAMA found that “individuals with COVID-19 were most infectious a few days before and after symptom onset.” However, according to data, rapid antigen tests often don't pick up COVID-19 infections until day 4. A 2022 study on Omicron in asymptomatic individuals found low accuracy of RATs (20-27%) and also found PCRs accuracy was only 40-48% amongst asymptomatic individuals. They concluded that “SARS-CoV-2 self-testing has limited value for asymptomatic individuals wishing to protect vulnerable persons and may even lead to a false sense of security. One should be aware of this, and better informed about other prevention options, such as physical distancing or mask use, on the other hand, all evaluated self-tests were highly specific. Therefore, self-testing regardless of symptoms is useful in other public health contexts because every positive test captured reduces the number of subsequent exposures. The high SARS-CoV-2 infection rate within 10 days of a negative RT-PCR test that we found in our study emphasizes the importance of re-testing over time, especially when symptoms develop, to reduce missed infections as much as possible.” A study on the accuracy of PCR tests in children and young adults found “that nearly 90% of children had negative nasopharyngeal RT-PCR samples, yet they seroconverted 6 weeks later, confirming infection”. A 2023 study shows other complex factors such as the variant and type of comparator a test brand uses (BinaxNow comparator was not as accurate for Omicron than it was for Delta; other brands using different comparators were about the same accuracy); the person's immune, vaccination status, and timing of last vaccine or infection also may play a role on when a person tests positive.
A person (whether vaccinated or not) should test:
If you have symptoms, test immediately.
The top 5 symptoms reported with Omicron infections are:
Note: These symptoms look like typical cold, flu and/or allergy symptoms, so if you think you might have a cold or new allergies, test immediately.
Test 1: Test again 1-2 days later if the first test is negative. Assume you have something infectious, wear a mask and stay home when possible.
Test 2: If the rapid test result is negative, isolate/quarantine (wear a mask any time you have to be around others) and repeat the test in 1-2 days.
Test 3: If you still have symptoms after two negative rapid tests, test a third time with a rapid test or get a PCR test. A PCR test will pick up lower viral levels (which may be a characteristic of Omicron infections), so get a PCR test if you have symptoms and repeatedly negative rapid tests.
B. If you were exposed, test as soon as possible and repeat 3-5 days after the exposure. For better accuracy, test every 2 days for a total of 3-4 tests, even if you don’t have symptoms.
C. Before travel, gathering or returning to school/work, test right before traveling/gathering/return and repeat 3-5 days after.
PCRs are higher accuracy but more expensive, Rapid Antigen Tests are less expensive but less accurate. Home molecular test kits are also available (Lucira COVID, Lucira COVID+flu, Metrix, PlusLife), which detect viral genetic material like PCR tests.
Note: Most at-home tests can be safely used past the date on the box. Check to see if your COVID-19 tests’ expiration dates have been extended on the FDA’s At-Home COVID-19 Test page. You can also see Australian Approved COVID Tests including Notes on Clinical Sensitivity for info on RAT Approval and Accuracy
Isolating
It is important to isolate properly to prevent transmission of COVID-19. There has been considerable confusion and debate in public health messaging regarding when and how long to isolate for, despite science that has consistently supported a minimum 14-day isolation period [10].
The Gold Standard Isolation guidance states: After isolating 14 days, before ending isolation, both of the following conditions must also be met:
1- No symptoms for three days AND
2- Two sequential negative PCR tests spaced 24-hours apart (each test should include samples taken from two sources). {see above testing section for more information on using other tests}
The above gold standard provides strong assurance that SARS-COV2 transmission will not take place from identified cases.
[10] A minimum 14 day isolation period, is considered the gold standard for isolation and is necessary for infection control from COVID-19. A 2022 study showed that among the SARS-CoV-2 Omicron variant infected patients, viral shedding continues for more than 10 days in 13.5% of all cases and 11% in symptom-free cases. Researchers also showed that determining infectiousness by symptoms is not accurate: “In 19% of the cases, the duration of shedding was longer than the duration of the symptoms. On day 5, four patients declared no more symptoms, although viruses were isolated by the culture. The rate of viral shedding among symptom-free cases was 58% on day 7, whereas they were 11% on day 10 and 5% on day 14”, showing infectious virus shedding continued up to 2 days after symptom resolution. A 2023 study showed a significant amount of infectious virus was detected in the exhaled breath of COVID-positive people for 8 days regardless of vaccination status, and including asymptomatic and mild cases. A person could therefore be infectious longer than the CDC guidelines, even in mild and asymptomatic cases, or cases when symptoms are improving or have stopped.
The CDC’s 2024 updated guidance strays from the research, where they recommend that people stay home and away from others until at least 24 hours after both their symptoms are getting better overall, and they have not had a fever (and are not using fever-reducing medication) and “encourages added precaution over the next five days after time at home, away from others, is over.” The guidance admits that others may still be contagious, saying: "Since some people remain contagious beyond the “stay-at-home” period, a period of added precaution using prevention strategies, such as taking more steps for cleaner air, enhancing hygiene practices, wearing a well-fitting mask, keeping a distance from others, and/or getting tested for respiratory viruses can lower the chance of spreading respiratory viruses to others.” However, precautions such as one-way masking, air filtration, and even vaccination work best in settings with reduced viral load. CDC’s 2024 guidance will increase the number of contagious people in spaces, and reduce the effectiveness of precautions.
COVID-19 Isolation policies should support a minimum of 14-day isolation to reduce viral density in public spaces so that the other methods of infection prevention have a greater chance at preventing infection.
Supporting Layers: Vaccines
Vaccines [11] may reduce risks of severe disease, hospitalization and death during the acute phase of infection thus providing biological protection for the individual. However, their effectiveness wanes over time, they don’t prevent infection or transmission, and they do not prevent long COVID. Also not all people are or can be vaccinated (some decide not to vaccinate due to their own risk-benefit analysis, some have medical contraindications such as allergic reactions) and not all who get vaccinated are significantly protected, (e.g. the elderly or immune-compromised). Thus, it is important to wear a mask whether vaccinated or not to prevent infection and transmission.
Figure 9: Vaccines: A Back-Up Layer to Reduce Some Forms of Risk
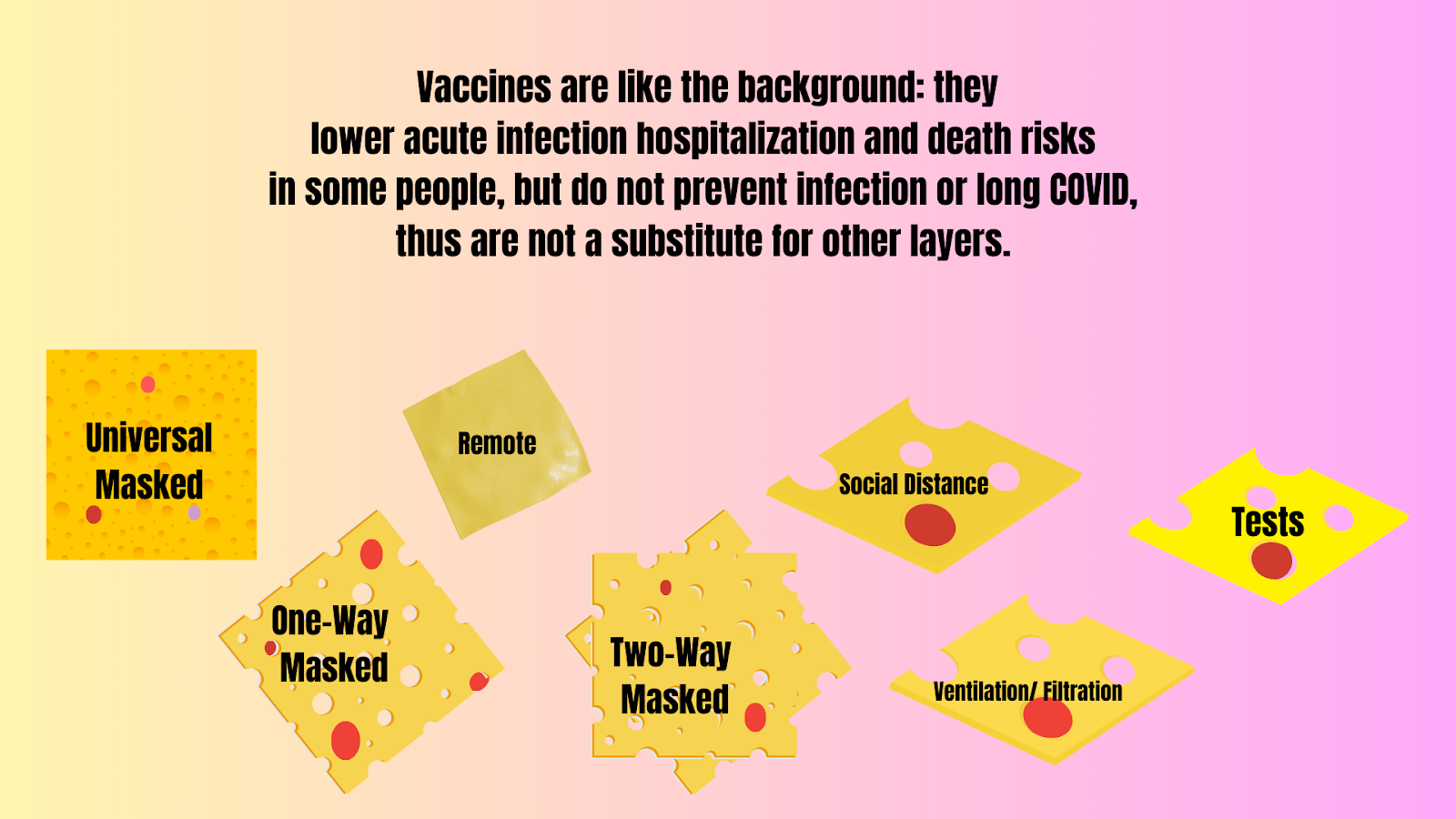
Vaccines are an additional layer to wearing a mask, not a substitution for it.
Individual responsibilities include staying educated about and up-to-date on vaccinations and available treatments, and seeking them when needed and appropriate, as well as maintaining other measures to prevent transmission.
[11] Vaccines: A 2022 study showed that 60-day vaccine efficacy of a second mRNA COVID-19 vaccine booster dose was 25.8% against infection, 60.1% against hospitalization, 89.6% against death, and 73.9% against the severe composite outcome of COVID-19–associated hospitalization or death. A 2023 study showed an estimated vaccine efficacy against hospitalization waned over time, showing 68% for a third dose 7 to 119 days after receipt, and 36% for a third dose 120 days or more after receipt. A 2024 study showed receipt of updated COVID-19 vaccine provided approximately 54% increased protection against symptomatic SARS-CoV-2 infection compared with no receipt of updated vaccine. A new 2024 study shows that the vaccine has been tied to a slight spike in certain conditions. Although the risks are much higher for infection from COVID-19, those who are able to shield and mask may weigh their risk benefit analysis differently. Vaccination does not prevent long COVID: Some studies show a modest reduction in long COVID amongst vaccinated individuals, but the reduction is not enough to lower risks to an acceptable level considering the nature of and lack of treatments for long COVID, and therefore is not considered a solution on its own. A 2022 study published in Nature, found a 15% reduction in long Covid amongst those vaccinated. The authors concluded that “vaccination before infection confers only partial protection in the post-acute phase of the disease; hence, reliance on it as a sole mitigation strategy may not optimally reduce long-term health consequences of SARS-CoV-2 infection.” A 2023 population-level analysis found vaccines reduced long COVID by 15-20%, with the authors concluding “Complementing vaccination campaigns with potential therapies, as well as further investing on prevention, might reduce the prevalence of long COVID and, consequently, should be considered for public health policies in the next future.” A 2023 Swedish study analysis found vaccine effectiveness against long COVID was 21% for one dose, 59% for 2 doses, and 73% for 3 or more doses, showing the importance of staying up-to-date on vaccinations, although it relied on diagnoses being made by primary care physicians in Sweden. A 2024 Lancet study found vaccines conferred 29-52% protection against long COVID. Barriers in defining, identifying, and diagnosing long COVID may be responsible for the variation in percentages for protective effect. Vaccine protection is not all or nothing: A 2023 study shows vaccines are much more effective in preventing transmission when the person inhales a smaller viral load. Masking can reduce inhaled viral load, which could in turn increase the vaccines’ ability to actually prevent infection.
Summary
In summary, it is important to not simply focus on using many layers, but to also pay attention to how these layers actually work and to choose complementary layers to provide true risk-reduction for you and others in the community. All are at risk for serious effects of COVID-19 and our actions affect those around us.
Using clear messaging about what really works is the first step in overcoming obstacles to technological development, related policies, and implementation, and to bringing these tools into our home, work, school, and business spaces.
For more information, visit World Health Network’s Guidelines for Individuals and Institutions.
For Information on School Safety see WHN’s Paths to Healthy Learning.
For information for Healthcare Professionals see Guidelines in Healthcare